Definition
Medial epicondylitis, often referred to as golfer’s elbow, involves tendinosis at the origin of the flexor-pronator mass. Despite its name, this condition is more commonly associated with racquet sports and manual labor.
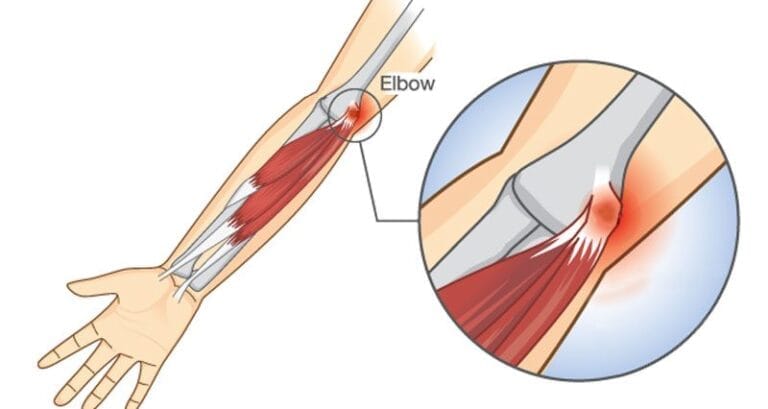
Anatomy
The common flexor-pronator origin is located primarily on the anterior aspect of the medial epicondyle. It includes the humeral head of the pronator teres (PT), flexor carpi radialis (FCR), flexor carpi ulnaris (FCU), and a small portion of the flexor digitorumsuperficialis (FDS). The palmaris longus also shares this origin, though it is not typically clinically significant.
Pathogenesis
Medial epicondylitis results from repetitive microtrauma, leading to an incomplete reparative response and tendinosis. This pathological state means the degenerative tendon cannot effectively heal itself. Medial epicondylitis can also be associated with medial collateral ligament instability, where the flexor-pronator mass attempts to dynamically stabilize the ulnohumeral joint. In such cases, ulnar neuropathy often coexists. The most commonly affected tendons are the PT and FCR, but any tendon in the common flexor-pronator origin can be involved.
Natural History
Most patients improve with conservative treatment. However, a higher percentage of patients with medial epicondylitis require surgical intervention compared to those with lateral epicondylitis.
Patient History and Physical Findings
Patients often report forearm pain rather than elbow pain, with significant inflammation potentially causing ulnar nerve irritation, resulting in symptoms like local irritability and distal numbness and tingling. Onset is usually insidious, though an inciting event may be recalled. Medial and lateral epicondylitis can coexist.
Examination Methods
- Palpation: Tenderness over the medial epicondyle is a universal finding.
- Resisted Pronation: Highly sensitive for medial epicondylitis.
- Range of Motion (ROM): A decreased ROM suggests intra-articular pathology such as arthritis.
- Resisted Wrist Flexion: Reproduction of symptoms supports the diagnosis.
- Tinel’s Sign: Tapping the ulnar nerve in the cubital tunnel may elicit a tingling sensation, indicating further nerve investigation is needed.
- Elbow Flexion Test: Flexing the elbow maximally and compressing the ulnar nerve just proximal to the cubital tunnel can provoke hand numbness or tingling, prompting further nerve investigation.
Imaging and Other Diagnostic Studies
- Plain Radiographs: May show calcifications at the flexor-pronator origin.
- Magnetic Resonance Imaging (MRI): Typically shows increased intratendon signal on T2-weighted sequences and possibly on T1-weighted sequences. Some patients may exhibit increased T2 signal in the medial epicondyle or anconeusedema.
- Electrophysiologic Testing: Electromyography and nerve conduction studies are recommended for patients with ulnar nerve symptoms, although sensitivity is low for mild ulnar neuropathy.
Differential Diagnosis
- Pronator syndrome
- Medial collateral ligament injury
- Ulnar neuropathy
- Arthritis
- Cervical radiculopathy
- Malingering
Nonoperative Management
Initial treatment includes avoiding painful activities and using nonsteroidal anti-inflammatory drugs (NSAIDs) and ice for symptomatic relief. Additional measures include:
- Daytime Wrist Bracing: For exertional activities.
- Physical or Occupational Therapy: To supervise and instruct on proper techniques and exercises to alleviate symptoms and improve function.