While elbow joint replacement is less common than knee, hip, or shoulder procedures, it offers comparable success in alleviating joint pain and restoring functionality for daily activities.
Whether you’re in the early stages of exploring treatment options or have already committed to elbow replacement surgery, this article aims to provide comprehensive insights into this effective procedure.
Anatomy:
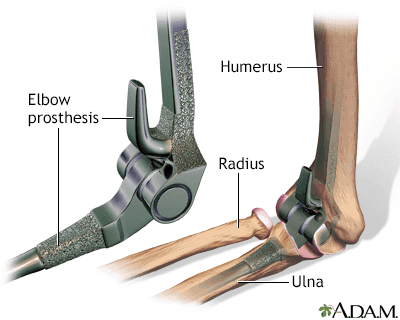
The elbow functions as a hinge joint and comprises three primary bones:
- The humerus (upper arm bone)
- The ulna (forearm bone on the pinky finger side)
- The radius (forearm bone on the thumb side)
Articular cartilage covers the surfaces of these bones where they meet, ensuring smooth movement and protecting against wear.
Additionally, a thin and soft synovial membrane tissue coats the elbow joint’s inner surfaces, producing a lubricating fluid that minimises friction during arm movement.
Muscles, ligaments, and tendons maintain the elbow joint’s stability.
Description:

During total elbow replacement surgery, the affected portions of the humerus and ulna are substituted with artificial components.
These prosthetic elbow joints typically have a metal and plastic hinge and two metal stems.
These items are designed to fit snugly within the bone’s canal, providing stability and support.
Various elbow replacements exist, with components available in different sizes to accommodate individual anatomical variations.
Partial elbow replacements may be considered for specific cases. Consulting with your physician is essential to determine the most suitable type of elbow replacement for your needs.
Cause:
Several conditions can contribute to elbow pain and disability, prompting patients and healthcare providers to consider elbow replacement surgery.
Rheumatoid Arthritis:
Rheumatoid arthritis is a type of inflammatory arthritis. This condition involves inflammation and thickening of the synovial membrane surrounding the joint.
Chronic inflammation could lead to cartilage damage and subsequent loss, resulting in pain and stiffness.
Osteoarthritis (Degenerative Joint Disease):
Osteoarthritis, often associated with ageing, is characterised by wear and tear on the joint. While more prevalent in individuals aged 50 and above, it can also affect younger individuals. The gradual cartilage erosion between elbow bones leads to bone-on-bone contact, resulting in stiffness and discomfort over time.
Posttraumatic Arthritis:
Posttraumatic arthritis can develop following a significant elbow injury. Fractures of the elbow bones or tears of surrounding tendons and ligaments can lead to gradual deterioration of the articular cartilage, resulting in pain and diminished elbow function.
Severe Fractures:
Severe fractures of the elbow bones are another prevalent indication for elbow replacement surgery. In cases where the elbow is severely shattered, reassembling the bone fragments can be challenging for surgeons.
interrupted blood supply to the bone fragments further complicates the situation, potentially necessitating elbow replacement surgery.
certain fractures may fail to heal adequately, prompting the need for elbow replacement to address persistent issues. Older individuals with osteoporosis, characterised by fragile bones, are particularly susceptible to severe elbow fractures.
Instability:
Elbow instability arises when the ligaments responsible for joint stability are compromised, leading to an increased risk of dislocation.
Chronic instability typically results from injury-induced ligament damage.
Preparing for Surgery:
Clinical Evaluation:
Before elbow replacement surgery, your orthopaedic surgeon may recommend scheduling a comprehensive physical examination with your family physician several weeks in advance. This evaluation is essential to ensure that you are in good health and will undergo the surgical procedure and subsequent recovery.
Patients with chronic medical conditions, such as heart disease, may also require evaluation by a specialist, such as a cardiologist, to assess their suitability for surgery.
Medication Management:
Discuss your medication regimen with your orthopaedic surgeon to determine if any adjustments are necessary before surgery.
Certain medications may need to be discontinued before the procedure to minimise risks.
For instance, over-the-counter medicines like aspirin, ibuprofen, and naproxen, known as non-steroidal anti-inflammatory drugs (NSAIDs), should be stopped at least two weeks before surgery due to their potential to increase bleeding.
Patients taking blood thinners will receive guidance from their primary care physician or cardiologist regarding discontinuing these medications before surgery.
medications prescribed for conditions like rheumatoid arthritis and other inflammatory disorders may require cessation before surgery. It is advisable to consult with your rheumatologist, as these medications often need to be discontinued before the surgical date.
Home Preparation:
Simple adjustments in your home environment before surgery can facilitate your recovery process. Accessing high shelves and cupboards during the initial weeks post-surgery may be challenging. Therefore, consider rearranging items to lower shelves beforehand for easier access after surgery.
Upon returning home from the hospital, assistance with daily tasks like dressing, bathing, cooking, and laundry will be necessary for a few weeks. If you do not have immediate assistance at home, you may be advised to undergo a brief rehabilitation period in a facility until you regain self-sufficiency.
Surgery Overview:
Before Your Operation:
You will be admitted to the hospital on the morning of your surgery. During your time in the preoperative preparation area, you will consult with an anesthesiologist to explore anaesthesia options. Depending on individual circumstances, some patients may be discharged on the same day as their surgery.
Surgical Procedure:
To access the elbow joint, your surgeon typically makes an incision at the back of the elbow.
Muscles are delicately shifted to reveal the bone, and any scar tissue and spurs are eliminated. Subsequently, replacement stems are implanted into the humerus and ulna bones and affixed using bone cement. These items are linked together via a hinge pin.
Some newer elbow replacements utilise the patient’s ligaments without a hinge mechanism, but this option is not suitable for everyone.
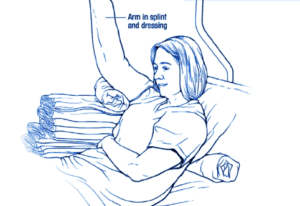
Following the closure of the wound, a dressing is administered to safeguard it throughout the healing period. Occasionally, a temporary drainage tube may be inserted into the joint to eliminate surgical fluid.
Implants:
Metal replacement parts are typically made of chrome-cobalt alloy or titanium with a polyethene liner. Bone cement used is usually polymethylmethacrylate.
Recovery:

The elbow is kept straight and elevated for the first few days after replacement
Antibiotics are administered to prevent infection, and most patients can resume solid food intake and mobility on the evening of surgery.
Pain Management:

Post-surgery pain is managed with prescribed medications, including opioids, non-steroidal anti-inflammatory drugs (NSAIDs), and local anaesthetics. Your doctor will tailor pain management to optimise relief and minimise opioid use, emphasising the importance of responsible medication usage to avoid dependency and overdose.
Rehabilitation:
A meticulously planned rehabilitation regimen is crucial for the success of elbow replacement surgery.
You will receive instruction on hand and wrist exercises to prevent stiffness and reduce swelling.
Gentle elbow range-of-motion exercises will be initiated as the incision heals.
Your doctor may prescribe therapy sessions or guide you on performing exercises independently.
Weight-bearing on the arm or resistance against hand pushing is typically restricted until approximately six weeks post-surgery.
Complications:
Your orthopaedic surgeon will discuss potential risks and complications associated with elbow joint replacement, encompassing those arising from the surgery and those that may develop over time.
Infection:
Infection is a potential risk with all surgical procedures, including elbow replacement. It can manifest in the wound or deep around the artificial components during hospitalisation or post-discharge and may even occur years later.
Antibiotics are typically administered to treat minor wound infections, while severe cases may necessitate additional surgery, potentially involving component removal.
Consult your doctor about the need for antibiotic prophylaxis before invasive procedures to mitigate infection risks.
Implant Issues:
Despite advancements in implant technology and surgical techniques, implant-related problems like wear, loosening, or component breakage may occur over time. Revision procedures may be required to address excessive wear or implant failure.
Why might I experience numbness in my hand following the procedure?
The proximity of several nerves to the elbow joint, particularly the ulnar nerve, poses a potential risk for postoperative numbness. The ulnar nerve traverses behind the elbow and through the joint is often relocated to facilitate a safe elbow replacement.
Nerves are susceptible; in some cases, their functionality may be compromised following transposition. Consequently, patients may experience numbness and tingling sensations in the ring and pinky fingers post-surgery.
While sensation typically returns to normal within weeks or months, permanent abnormal feelings can occur.
Although rare, ulnar nerve damage may result in hand weakness or clumsiness after surgery.
Nerve Injury:
While rare, nerve injuries near the joint replacement site may occur during surgery. These injuries typically resolve over time without intervention.
Wound Healing:
Careful wound care is essential to prevent complications associated with wound healing.
Long-Term Outlook:
Total elbow replacement surgery generally improves quality of life, reduces pain, and enhances motion, strength, and functionality. Patients typically regain the ability to perform daily activities, but they should avoid certain high-risk activities and heavy lifting to prevent implant-related complications.
Security Screening:
Travelling with a metal implant may trigger security screenings at airports. Inform security personnel about your elbow replacement to facilitate the screening process. While this does not alter screening requirements, it helps security personnel understand the nature of the alarm and may involve additional screening methods, such as wand scanning or visual inspection of the scar.
Research:
Ongoing research aims to enhance implant durability and prevent implant failure. research focuses on understanding joint degeneration in patients with rheumatoid arthritis, with newer medications aimed at slowing disease progression and potentially averting the need for elbow replacement surgery.