Arthritis is characterised by inflammation in one or more joints. Symptoms include pain, swelling, and stiffness.
Arthritis could impact any joint in the body, but it tends to be more prevalent in the knee.
Knee arthritis frequently impedes daily tasks like walking or climbing stairs, resulting in notable disability and work absenteeism for numerous individuals.
The top two types of arthritis are osteoarthritis and rheumatoid arthritis, encompassing over 100 variations. While arthritis is mainly seen in adults, specific types may also affect children.
While arthritis cannot be cured, numerous treatment options are available to help alleviate pain and enable individuals to remain active.
Knee Anatomy
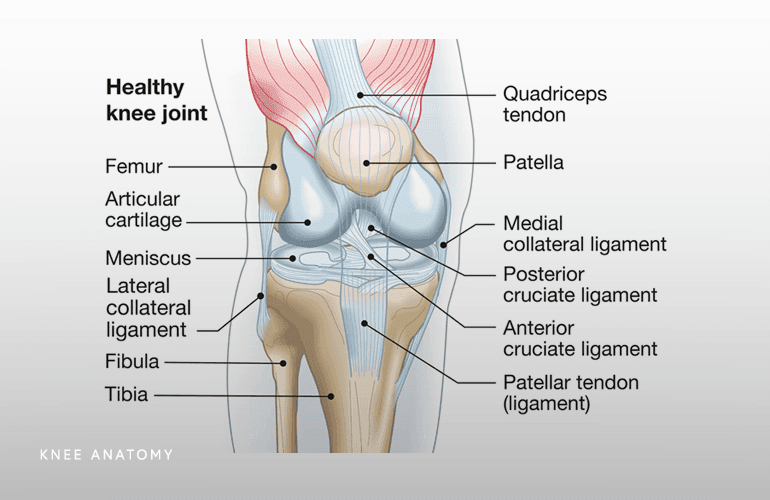
The knee, the largest and most robust joint in the body, comprises the lower portion of the femur (thighbone), the upper portion of the tibia (shinbone), and the patella (kneecap).
Articular cartilage, a smooth and slick substance, covers the ends of these three bones, providing protection and cushioning during knee movements.
Two wedge-shaped cartilage pieces known as meniscus are shock absorbers between the thigh bone and shinbone.
These resilient structures help cushion the joint and maintain its stability.
A thin lining called the synovial membrane surrounds the knee joint. It secretes fluid to lubricate the cartilage and minimise friction.
Description
The primary types of arthritis affecting the knee include osteoarthritis, rheumatoid arthritis, and posttraumatic arthritis.
Osteoarthritis:
Osteoarthritis is the most prevalent form of knee arthritis. It is characterised by degeneration and wear-and-tear of the joint and typically affects individuals aged 50 and above, although it can also occur in younger individuals.
In osteoarthritis, the cartilage within the knee joint gradually deteriorates, leading to fraying and roughening of the cartilage surface.
This reduces the protective space between the bones, potentially causing bone-on-bone contact and the formation of painful bone spurs.
The progression of osteoarthritis is typically gradual, with worsening pain over time.
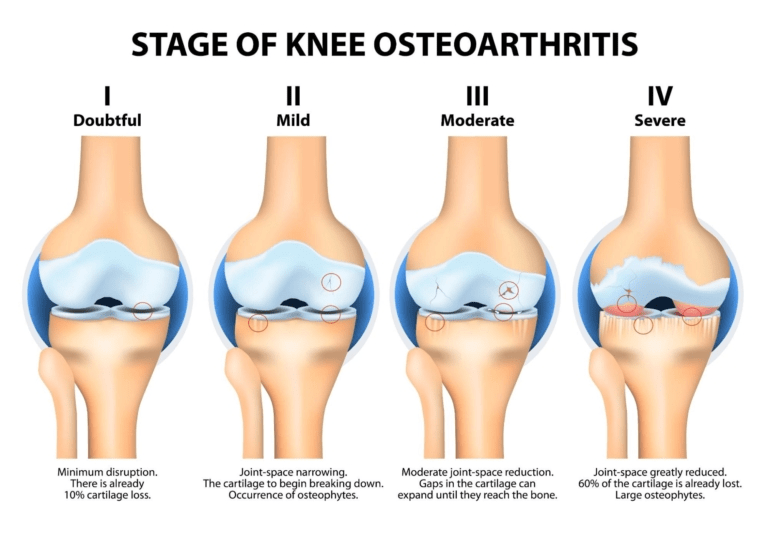
Stage 1 – Minor:
In stage 1 of osteoarthritis (OA), patients experience minimal wear and tear, often without noticeable pain or discomfort.
Stage 2 – Mild:
Stage 2 reveals more evident wear and tear and the growth of bone spurs in diagnostic images or X-rays. While the space between the bones remains relatively normal, individuals may begin to feel joint pain. Stiffness and discomfort, particularly after periods of inactivity or exercise, are common symptoms.
Stage 3 – Moderate:
Stage 3, categorised as “moderate”, presents noticeable erosion of cartilage surfaces between bones, narrowing the gap between bones and increased roughness of joint surfaces. Joint inflammation intensifies, resulting in more frequent pain, worsened stiffness, and potential popping or snapping sounds during movement.
Stage 4 – Severe:
Considered severe, stage 4 depicts a significant reduction in joint space between bones, with cartilage wearing through, resulting in pronounced stiffness.
The breakdown of cartilage triggers chronic inflammation, decreased synovial fluid, and heightened friction, causing considerable discomfort during joint movement.
More bone spurs exacerbate pain, making routine activities like walking and stair descent challenging. Surgery is often recommended at this stage.
Causes of Knee Osteoarthritis:
The precise reasons why certain individuals develop osteoarthritis (OA) in their knees remain unclear.
Several factors could heighten the risk of its occurrence.
Risk Factors for Knee Osteoarthritis:
Age:
While OA can manifest at any age, it is prevalent among older adults, particularly those over 50.
Gender:
Women exhibit a higher likelihood of knee OA compared to men. Research suggests that approximately 19% of women experience knee OA, contrasted with 13.5% of men.
Obesity:
Body weight directly impacts the load borne by the lower limb joints during weight-bearing activities. Excess weight places added stress on your knees, while fat cells produce proteins that may induce inflammation in and around the joints.
Injuries:
Any previous knee injury, regardless of age, elevates the risk of developing knee OA.
Excessive Strain:
Overloading the knee due to occupational demands or engaging in excessive high-impact exercises, such as prolonged running or participation in high-impact sports, can heighten the risk of OA.
Genetics:
A hereditary predisposition exists for OA development. Individuals with family members affected by OA are at an increased risk.
Bone Deformities:
Altered bone or joint alignment, as well as any bony abnormalities, raise the likelihood of developing OA.
Certain Metabolic Diseases:
Conditions like diabetes and hemochromatosis, characterised by excess iron in the blood, have been associated with OA development.
Types of Arthritis Affecting the Knee
Rheumatoid Arthritis:
Rheumatoid arthritis is a chronic condition that targets multiple joints in the body, including the knee joint. It typically affects both sides of the body symmetrically.
In rheumatoid arthritis, the synovial membrane surrounding the knee joint becomes inflamed, leading to pain and stiffness in the knee.
This condition is classified as an autoimmune disease, where the body’s immune system mistakenly attacks its own tissues, resulting in damage to normal tissues such as cartilage and ligaments, as well as bone softening.
Posttraumatic Arthritis:
Posttraumatic arthritis develops following a knee injury, such as a fracture that damages the joint surface, eventually leading to arthritis years after the initial injury. Meniscal tears and ligament injuries can also contribute to knee instability and additional wear on the joint, eventually leading to arthritis.
Symptoms:
Arthritic knee joints often exhibit pain and inflammation. Pain may develop gradually over time or suddenly. Additional symptoms may include:
- Stiffness and swelling in the joint make it challenging to bend or straighten the knee.
- Increased pain and swelling in the morning or after periods of rest.
- Aggravated pain during vigorous activity.
- Disruption of smooth joint motion due to loose cartilage fragments, leading to joint locking, clicking, snapping, or grinding noises (crepitus).
- Weakness or buckling sensations in the knee due to pain.
- Many individuals with arthritis notice heightened joint pain in response to changes in weather conditions.
Medical Evaluation Process
During your medical consultation, your doctor will discuss your symptoms and medical background, perform a physical assessment, and potentially recommend diagnostic examinations like X-rays or blood analyses.
Physical Assessment
Throughout the physical evaluation, your doctor will observe for:
- Swelling, warmth, or redness in the joints
- Tenderness surrounding the knee area
- Assessment of both passive (aided) and active (self-directed) range of motion
- Examination of joint stability
- Identification of crepitus (a grinding sensation within the joint) during movement
- Evaluation of pain response under weight-bearing conditions
- Assessment of gait abnormalities
- Detection of any muscle, tendon, or ligament injuries related to the knee
- Exploration of potential involvement of other joints, which may indicate rheumatoid arthritis
Imaging Procedures
X-rays:
These imaging techniques offer detailed visuals of dense structures like bones, aiding in distinguishing between various arthritis types. X-rays of an arthritic knee may reveal joint space narrowing, bone alterations, and the development of bone spurs (osteophytes).
Additional Assessments:
In some cases, a magnetic resonance imaging (MRI) or computerised tomography (CT) scan may be necessary to comprehensively assess the condition of knee bones and soft tissues.
Diagnostic Blood Tests
Your doctor may also advise undergoing blood tests to ascertain the type of arthritis you are experiencing. Particularly in cases like rheumatoid arthritis, these blood examinations are essential for an accurate diagnosis.
Treatment Options
Although there is no cure for arthritis, there are numerous treatment approaches available to alleviate the pain and disability associated with it.
Nonsurgical Treatment
Initial treatment for knee arthritis typically involves nonsurgical methods. Your healthcare provider may suggest various options:
Lifestyle Adjustments:
Changing your daily routines can safeguard your knee joint and slow the progression of arthritis.
Exercise:
Physical activity can improve pain and function for osteoarthritis sufferers. Transitioning from high-impact to lower-impact exercises can allow for activity while reducing knee stress.
Weight Loss:
Shedding excess weight can lessen stress on the knee joint, resulting in reduced pain and improved function.
Physical Therapy:
Tailored exercises can enhance flexibility, range of motion, and muscle strength in the leg.
Assistive Devices:
Tools like canes or knee braces can aid in stability and function, particularly if arthritis is localised.
Other Remedies:
Applying heat or ice or using elastic bandages can relieve knee pain.
Medication Options
Various medications are effective in treating knee arthritis, with your doctor guiding you on the safest and most suitable options:
Pain Relievers:
Over-the-counter pain relievers and anti-inflammatory medications are commonly recommended to manage arthritis pain. However, they may carry side effects and interact with other medications.
Nonsteroidal Anti-Inflammatory Drugs (NSAIDs):
NSAIDs, like ibuprofen and naproxen, are available over-the-counter or by prescription. They offer pain relief and reduced inflammation.
Topical NSAIDs:
These medications, applied directly to the skin, can be effective for knee pain relief, especially for those unable to tolerate oral NSAIDs.
Corticosteroid Injections:
Injecting cortisone into the joint can relieve pain and reduce inflammation, though the effects may not be long-lasting.
Disease-Modifying Anti-Rheumatic Drugs (DMARDs):
Drugs like methotrexate or biologics can slow the progression of rheumatoid arthritis.
Supplements:
Glucosamine, chondroitin sulfate, and other dietary supplements may alleviate pain, although their effectiveness is not fully supported by evidence.
Alternative Therapies
While unproven, some alternative therapies may be worth considering under the supervision of a qualified practitioner:
Acupuncture: T
his practice involves using fine needles to stimulate specific body areas, potentially relieving arthritis pain.
Magnetic Pulse Therapy:
Painless therapy that applies a pulsed signal to the knee within an electromagnetic field.
Biologic Treatments:
Platelet-rich plasma (PRP) and stem cell injections involve reintroducing cells from the body into the affected joint.
While these treatments hold promise, their efficacy in treating osteoarthritis remains to be fully validated through clinical studies.
Surgical Interventions
In cases where arthritis-related pain and disability persist despite nonsurgical approaches, surgery may be recommended. It’s essential to understand the potential risks and complications associated with various knee procedures, which your doctor will discuss with you beforehand.
Arthroscopy:
This minimally invasive procedure uses small incisions and thin instruments to diagnose and treat joint issues. While not commonly used for arthritis, arthroscopy may be employed to address concurrent degenerative meniscal tears.
Cartilage Grafting (Cartilage Restoration):
Healthy cartilage tissue from another part of the knee or a tissue bank may be used to fill defects in the articular cartilage. This option is typically considered for younger patients with localised cartilage damage.
Synovectomy:
Removal of the inflamed joint lining can help alleviate pain and swelling associated with rheumatoid arthritis.
Osteotomy:
In knee osteotomy, the tibia or femur is surgically cut and reshaped to redistribute pressure within the knee joint. This procedure is suitable for individuals with early-stage osteoarthritis affecting one side of the knee, aiming to relieve pain and enhance function.
Total Knee Replacement or Partial Knee Replacement (Arthroplasty):
This involves removing damaged cartilage and bone or replacing them with artificial joint surfaces made of metal or plastic to restore knee function.
Rehabilitation
The recovery process following knee surgery for arthritis varies depending on the procedure. Your doctor may advise physical therapy to rebuild knee strength and improve range of motion. Depending on the surgery, you might require a knee brace or assistance from crutches or a cane for a period.
Typically, surgery alleviates pain and enhances the ability to engage in everyday activities more comfortably.
Knee Rehabilitation Exercises
For safety and effectiveness, it’s crucial to perform this program under the supervision of your doctor. Consult your doctor and physiotherapy to determine the most suitable exercises to meet your rehabilitation objectives.
Whether recovering from injury or surgery, an exercise regimen is vital in restoring functionality and facilitating a return to daily activities. Adhering to a carefully structured conditioning program can also aid in resuming sports and recreational pursuits.
Heel Cord Stretch
Target Muscles: Gastrocnemius-soleus complex
Sensation: You should feel the stretch in your calf and heel.
Equipment Required: None
Instructions:
- Stand facing a wall with the unaffected leg forward, slightly bent at the knee. Your affected leg should be straight and positioned behind you, with the heel flat and toes pointing inward slightly.
- Keep both heels grounded and gently push your hips forward toward the wall.
- Hold this position for 30 seconds, then relax for 30 seconds. Repeat.
Repetitions:
Perform 2 sets of 4 repetitions.
Frequency:
Practice 6 to 7 days per week.
Tip:
Avoid arching your back.
Half Squats
Target Muscles:
Quadriceps, Gluteus, Hamstrings
Sensation:
You should feel this exercise working the front and back of your thighs and buttocks.
Equipment Required:
As the exercise becomes more accessible, gradually increase resistance by incorporating hand weights. Start with 5-pound weights and progress to heavier weights as tolerated.
Instructions:
- Stand with your feet shoulder-width apart. Your hands can rest on the front of your thighs or extend in front of you for balance. For additional support, hold onto the back of a chair or wall.
- Maintain an upright posture and slowly lower your hips about 10 inches, mimicking sitting on a chair.
- Ensure your weight is evenly distributed on your heels, and hold the squat for 5 seconds.
- Push through your heels to return to the standing position.
Repetitions:
Perform three sets of 10 repetitions.
Frequency:
Practise this exercise 4 to 5 days per week.
Tip:
Avoid leaning forward at the waist during the movement.

Leg Extensions
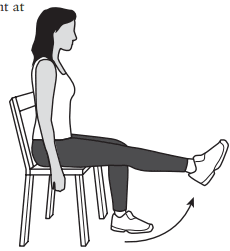
Target Muscles:
Quadriceps
Sensation:
You should feel this exercise engaging the front of your thigh.
Equipment Required:
As the exercise becomes easier, gradually increase resistance by incorporating ankle weights. Begin with a 5-pound weight and progress to heavier weights up to 10 pounds. Alternatively, if available, this exercise can be performed on a weight machine at a fitness centre, with guidance from a fitness assistant.
Instructions:
- Sit upright on a chair or bench.
- Tighten your thigh muscles and slowly straighten and raise your affected leg as high as possible.
- Hold this extended position for 5 seconds, contracting your thigh muscles, then relax and lower your foot back to the floor. Repeat the movement.
Repetitions:
Complete 3 sets of 10 repetitions.
Frequency:
Practise this exercise 4 to 5 days per week.
Tip:
Avoid using momentum or swinging your leg to lift it higher; focus on controlled movements.
Leg Presses

Target Muscles: Quadriceps, Hamstrings
Sensation:
You should feel this exercise engaging the front of your hip, as well as the front and back of your thigh.
Equipment Required:
An elastic stretch band of comfortable resistance is ideal for this exercise. As you progress, gradually increase the resistance level. Avoid using ankle weights. Alternatively, if available, this exercise can be performed on a weight machine at a fitness center, with guidance from a fitness assistant.
Instructions:
- Place the centre of the elastic band at the arch of your foot and hold the ends in each hand. Lie on the floor with your elbows bent.
- Engage the thigh muscle of your affected leg and bring your knee toward your chest.
- Flex your foot and slowly straighten your leg directly in front of you, pushing against the resistance of the elastic band.
- Hold this extended position for 2 seconds, then relax and lower your leg back to the floor. Repeat the movement.
Repetitions:
Complete 3 sets of 10 repetitions.
Frequency:
Perform this exercise 4 to 5 days per week.
Tip:
Maintain tight abdominals throughout the exercise to stabilize your core.
Supine Hamstring Stretch

Muscles Targeted:
Hamstrings
Sensation:
You should feel a stretch along the back of your thigh and behind the knee.
Equipment Needed:
None
Instructions:
- Lie on your back with both legs bent on the floor.
- Lift one leg off the floor and bring the knee toward your chest.
- Clasp your hands behind your thigh below the knee.
- Straighten your leg and gently pull it toward your head until you feel a stretch. If reaching behind your leg is difficult, use a towel looped around your thigh for assistance.
- Hold the stretched position for 30 to 60 seconds.
- Repeat the stretch with the opposite leg.
Repetitions:
Perform this stretch 2 to 3 times.
Frequency:
Include this stretch in your routine 4 to 5 days weekly.
Tip:
Avoid pulling directly on your knee joint. Instead, focus on gently stretching the hamstring muscles.