National Tennis Elbow Guidance by British Elbow and Shoulder Society
Introduction
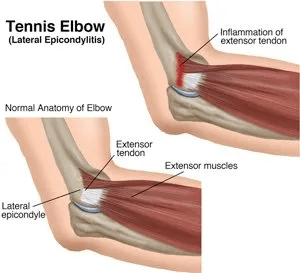
The national guidelines for lateral elbow tendinopathy, also known as tennis elbow, were spearheaded by Professor Imam and a team of prominent shoulder and elbow surgeons in the UK. This prevalent condition manifests as pain on the outer aspect of the elbow, which may extend to the forearm and hinder tasks involving gripping or delicate hand movements. Diagnosis primarily relies on discussing symptoms and conducting a thorough examination by a medical professional. Management of this condition necessitates a collaborative approach between doctors and patients, emphasising active listening, clear communication, and mutual respect for treatment preferences.
Key Points:
Around 4 to 7 out of every 1000 people get lateral elbow tendinopathy yearly.
It’s most common in people aged 35 to 54.
While it often gets better independently, some people have ongoing issues.
Treatment focuses on relieving pain and improving function, with decisions made between the patient and their doctor.
Guidelines:
Physiotherapy is a strongly recommended treatment.
Self-management strategies like stretching exercises and pain-relieving creams can help.
Doctors usually diagnose it based on symptoms and examination without needing X-rays or specialist scans.
Treatment options in primary care include painkillers, physiotherapy, and education about self-care.
If symptoms don’t improve in primary care, a referral to specialist care may be necessary.
Research and Future Directions:
Researchers are looking into the best ways to treat elbow tendinopathies, both with and without surgery.
They’re also working on defining the most important outcomes to measure in studies about this condition.
In the future, studies should compare different treatments for lateral elbow tendinopathy (LET) to either a fake treatment or no treatment at all. These studies should also follow patients for at least 12 months to see how well the treatments work over time.
There are several important questions that still need answers about treating LET:
1. Does using imaging tests, like MRI scans, help doctors treat LET better?
2. Is physiotherapy helpful for patients who’ve had surgery for LET?
3. Does physiotherapy work for patients who’ve had symptoms of LET for more than a year?
4. Is surgery better than no treatment or a fake treatment for patients who don’t get better with non-surgical treatments?
5. Is a treatment called PRP injection better than a fake treatment for LET?
Currently, research suggests that physiotherapy might help reduce pain and improve function in the short term for LET. However, more studies are needed to understand the long-term effects and safety of treatments like corticosteroid injections and surgery.
This table presents treatment recommendations for lateral elbow tendinopathy (LET) in a patient-friendly format, focusing on what patients should consider and avoid when managing their condition.
| Treatment Recommendation | Level of Recommendation |
| Try physiotherapy for LET pain relief. | Strong |
| Avoid corticosteroid injections for LET treatment. | Strong |
| Skip shockwave therapy for LET treatment. | Strong |
| Consider imaging if unsure about LET diagnosis. | Conditional neutral |
| Imaging choice depends on patient and local factors. | Conditional neutral |
| Physiotherapy may help if LET symptoms last over 12 months. | Conditional neutral |
| Physiotherapy can aid recovery after LET surgery. | Conditional neutral |
| PRP treatment for LET might not be better than placebo. | Conditional neutral |
| Dry needling for LET might not offer more benefit than placebo. | Conditional neutral |
| Surgery for LET might not be more effective than placebo. | Conditional neutral |
| Surgery can be done with open or arthroscopic techniques. | Conditional neutral |
| Avoid autologous blood injection for LET treatment. | Conditional |
| Orthotics might help LET, but benefits are uncertain. | Conditional |
| Use NSAIDs for short-term LET pain relief, preferably topical to avoid stomach issues. | Conditional |
Summary of Recommendations:
- Physiotherapy Treatment for LET: Strongly Recommended
- Corticosteroid Injection for LET: Not Recommended
Review Question:
Is there a role for corticosteroid injection in the treatment of LET?
Evidence Summary:
Studies comparing patient information and wait-and-see approaches with placebo saline injection or sham ultrasound therapy as ‘no intervention’ comparators suggest that physiotherapy offers significant short-term improvement in overall outcome for LET, with some reduction in pain and disability in the long term.
uncertainty remains due to the need for more high-quality studies with validated outcome measures for mid- and long-term outcomes.
Evidence from meta-analyses and RCTs indicates that corticosteroid injections should not be used for LET treatment.
Despite some initial pain improvement, the long-term outcomes are worse compared to placebo or no intervention. This recommendation is based on moderate to very low-quality evidence, with concerns about bias and inconsistency among studies.
Recommendations and Evidence for Lateral Elbow Tendinopathy (LET)
- Imaging for LET Management:
- Consider imaging for LET when the diagnosis is uncertain.
- No evidence supports or refutes its use.
- Ultrasound vs. MRI for LET Management:
- There is no difference between ultrasound and MRI in LET management.
- The choice depends on the patient and local factors.
- Non-Steroidal Drugs for LET Management:
- Topical or oral NSAIDs can relieve short-term LET pain.
- Evidence quality for topical NSAIDs is low.
- Physiotherapy for LET Beyond 12 Months:
- There is no clear evidence for physiotherapy in LET beyond 12 months.
- Consider physiotherapy if not previously offered.
- Post-Operative Physiotherapy for LET:
- No evidence supports or refutes post-operative physiotherapy.
- Patients may be offered physiotherapy after surgery.
- PRP for LET Treatment:
- PRP may not be more effective than a placebo for LET.
- Evidence quality could be a lot higher.
- Autologous Blood Injection for LET:
- Autologous blood injection offers no significant benefit over saline infusion.
- More research comparing ABI to a trustworthy placebo is needed.
- Dry-Needling for LET Treatment:
- No evidence supports dry-needling over placebo for LET.
- Limited evidence suggests short-term pain improvement.
- Orthotics for LET Management:
- Orthotics may be offered, but evidence of benefit is lacking.
- Immediate grip strength improvement was noted in some studies.
- Extracorporeal Shock Wave Therapy (ESWT) for LET:
- ESWT should not be used for LET treatment.
- Moderate evidence shows no improvement in pain or function.
- Surgery for LET:
- Surgery offers no benefit over a placebo for LET.
- Limited evidence due to methodological flaws.
- Arthroscopic vs. Open Surgery for LET:
- There is no difference between arthroscopic and open surgery outcomes.
- More evidence is needed due to the small sample sizes.
- Novel Therapies for LET:
- Novel therapies like PUT, DPT, iontophoresis, TAE, and BMAI lack evidence.
- It is only recommended within clinical trials due to very low-quality evidence.
- Risk Factors for LET Recurrence:
- Older age, short recovery periods, and chronic LET increase recurrence risk.
- Corticosteroid injections and poor adherence to management plans also contribute.
To effectively manage lateral elbow tendinopathy (LET), measuring specific health-related aspects is crucial. These include:
- Patient’s Rating of Condition: How the patient perceives their condition.
- Participation in Life Activities: Ability to engage in daily tasks, work, and sports.
- Pain on Activity/Loading: Pain experienced during movement or loading.
- Function: Overall functionality and movement capability.
- Psychological Factors: Emotional and mental aspects influencing recovery.
- Physical Function Capacity: The ability to perform physical tasks.
- Disability: Impairment affecting daily life and activities.
- Quality of Life: General well-being and satisfaction with life.
- Pain Over a Specified Time: Monitoring pain levels over a defined period.
A core outcome set has been developed to ensure consistency in measuring these aspects. The Patient-Reported Tennis Elbow Evaluation (PRTEE) questionnaire is recommended for assessing disability.
Other interim recommendations include using PRTEE sub-scales, time off work, pain-free grip strength, and a numerical rating scale for pain on gripping to determine function, pain, activity participation, physical capacity, and pain during activity/loading.
These recommendations are based on a systematic review and international consensus involving clinicians, researchers, and patients. By using standardised tools, healthcare providers can better understand and address the needs of individuals with LET, ultimately improving treatment outcomes.