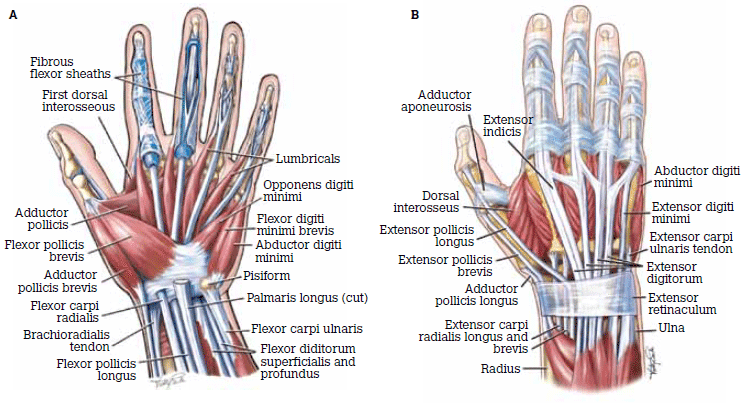
Anatomy of the hand
Introduction to De Quervain Syndrome
De Quervain syndrome, also known as de Quervain’s tenosynovitis, is a painful condition affecting the tendons on the thumb side of the wrist. This syndrome can significantly impact hand function, causing pain and tenderness that extends into the lower arm. Often resulting from repetitive hand or wrist movements, de Quervain’s syndrome leads to inflammation within the tendon sheath that surrounds two crucial tendons responsible for thumb movement.
Causes and Risk Factors
The exact causes of de Quervain’s syndrome are not fully understood, but it is closely linked to repetitive thumb and wrist motion activities. These include various occupational and recreational activities, such as gardening, typing, and certain sports. Additionally, pregnancy and rheumatoid arthritis are known risk factors, possibly due to hormonal fluctuations and increased fluid retention in the former and inflammation in the latter.
Signs and Symptoms
The primary symptoms of de Quervain syndrome include:
- Pain and Swelling: Occurring on the thumb side of the wrist, which may worsen with activity.
- Tenderness: At the base of the thumb, accompanied by swelling that can make it difficult to grasp or pinch objects.
- Crepitus: A crunching sensation when moving the thumb.
- “Sticking” sensation: When moving the thumb due to the inflamed tendons.
When considering differential diagnoses based on imaging for de Quervain syndrome, it’s essential to assess for other conditions that might present with similar symptoms:
- Tenosynovitis Related to Inflammatory Arthropathies: This condition, such as rheumatoid arthritis, involves inflammation of the tendon sheaths and can mimic the symptoms of de Quervain syndrome. It typically affects multiple joints and tendons rather than being localised.
- Intersection Syndrome: This syndrome occurs more proximally compared to de Quervain syndrome. It involves inflammation or irritation where the muscles and tendons of the forearm cross over each other approximately 4 cm proximal to Lister’s tubercle on the radius.
- Peritendinitis of the First and Second Extensor Compartment Tendons: This involves inflammation where the tendons of the first and second extensor compartments cross each other. It’s also located approximately 4 cm proximal to Lister’s tubercle, similar to intersection syndrome but affecting the tendons differently.
Non-Surgical and Surgical Treatments
Before considering surgery, non-surgical methods such as rest, ice application, and anti-inflammatory medications (e.g., ibuprofen) are recommended to alleviate symptoms. For persistent cases, corticosteroid injections may be administered to reduce inflammation quickly, although they come with risks like tendon weakening.
If symptoms persist despite these measures, surgical intervention may be considered. The surgical approach typically involves a “surgical release,” which reduces the compartmental pressure on the tendons, allowing them to move freely without pain.
Rehabilitation Exercises for De Quervain Syndrome
Rehabilitation exercises are crucial in managing de Quervain syndrome as they help reduce pain, increase mobility, and strengthen the muscles around the wrist and thumb. Here is a more detailed description of each recommended exercise:
1. Isolated Thumb MP-Joint Extensor Stretch
- Purpose: This exercise aims to stretch the muscles and relieve tension around the thumb’s metacarpophalangeal (MP) joint.
- How to Perform:
- Extend your arm in front of you with the palm facing up.
- Using your opposite hand, gently press the thumb downwards towards the wrist until a stretch is felt along the thumb side of the wrist and forearm.
- Hold this position for 15-30 seconds.
- Repeat the stretch 2-4 times, ensuring there is no pain. If pain occurs, reduce the intensity of the stretch

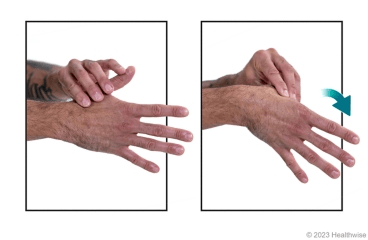
2. Finkelstein Stretch
- Purpose: Specifically targets the tendons affected by de Quervain’s syndrome to reduce tightness and increase flexibility.
- How to Perform:
- Make a fist with the thumb tucked inside the fingers.
- Bend your wrist towards your little finger.
- A stretch should be felt on the thumb side of the wrist.
- Hold for 15-30 seconds and gently release.
- Perform this stretch 2-4 times, taking care not to exacerbate the pain.
3. Thumb Flexion and Extension
- Purpose: Improves the range of motion and flexibility of the thumb.
- How to Perform:
- Place the affected hand palm-down on a table.
- Slowly bend the thumb towards the palm, attempting to touch the base of the small finger.
- Hold the position briefly, then extend the thumb back to the starting position.
- Repeat the motion 8-12 times, ensuring smooth, pain-free movement.
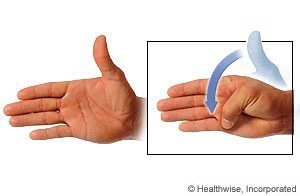
4. Thumb Adduction and Abduction
- Purpose: Strengthens the muscles that move the thumb away from and towards the hand, enhancing overall thumb mobility.
- How to Perform:
- Start with the hand open, thumb extended outward.
- Slowly move the thumb across the palm towards the base of the little finger (adduction), and then back to the starting position (abduction).
- Perform 8-12 repetitions, maintaining a relaxed wrist and ensuring each movement is pain-free.

5. Resisted Radial Deviation
- Purpose: Strengthens the wrist muscles, specifically those supporting radial deviation, which involves moving the wrist towards the thumb.
- How to Perform:
- Sit with the forearm resting on your thigh for stability, wrist extended just beyond the knee.
- Hold one end of a resistance band in your hand, with the other end secured underfoot.
- Move the wrist upwards, lifting against the resistance of the band, then slowly return to the starting position.
- Repeat 8-12 times, focusing on controlled movements to avoid jerking, which could exacerbate symptoms.
These exercises should be performed gently and increased in intensity only as comfort allows. Consistent practice is key to achieving the best results in managing symptoms of de Quervain syndrome. Always consult with a healthcare professional before starting a new exercise regimen to ensure it’s appropriate for your specific condition.