Introduction
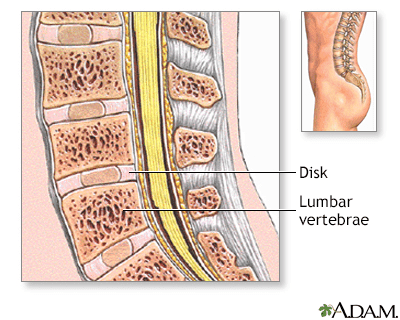
Spinal fusion surgery is frequently performed to stabilise or relieve pain in the neck or back. This procedure fuses unstable or painful spinal bones into a single, solid bone, requiring additional bone grafts to facilitate healing.
The success of bone formation hinges on three main components:
- Stability (often provided by screws, rods, and plates).
- Cells generate bone.
- Proteins to stimulate growth.
- A scaffold for bone attachment.
Types of Bone Grafts
Autograft

- Definition: Bone taken from the patient’s body, typically the iliac crest.
- Advantages: High compatibility, contains essential cells and proteins, no risk of disease transmission.
- Disadvantages: Limited supply, potential for pain and complications at the harvest site, risk of infection or bleeding.
Autografts have traditionally been used due to their effectiveness, but newer technologies and techniques have reduced their frequency of use, particularly in high-risk patients. Minimally invasive harvesting techniques have been developed to minimise donor site trauma and pain.
Local Bone Autograft
- Definition: Recycled bone from the surgical site.
- Advantages: There are no additional incisions, no hip pain, and the patient’s bone is preserved, which ensures compatibility and availability of necessary cells and proteins.
- Disadvantages: Limited quantity due to the small size of spinal bones.
This method effectively utilises the patient’s bone without additional surgical sites, reducing the risk of complications and pain associated with bone harvesting from other locations.
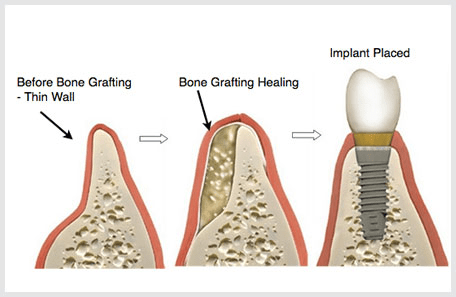
Allograft Bone
- Definition: Donor or cadaver bone processed to remove cells and reduce immune response.
- Advantages: It is available in various sizes and shapes, avoids additional surgery, and acts as a scaffold for new bone growth.
- Disadvantages: It does not form new bone independently, has rare disease transmission, and has lower bone healing potential than autografts.
Allografts have been successfully used for years, offering an alternative to autografts without the associated harvest site complications.
Allograft with Stem Cells
- Definition: Allograft bone combined with donor stem cells.
- Advantages: Enhanced healing and fusion rates, minimal rejection risk.
- Disadvantages: Higher cost, limited long-term data, often requires combination with other graft materials.
Combining stem cells with allografts can improve fusion outcomes, though more research is needed to establish long-term efficacy.
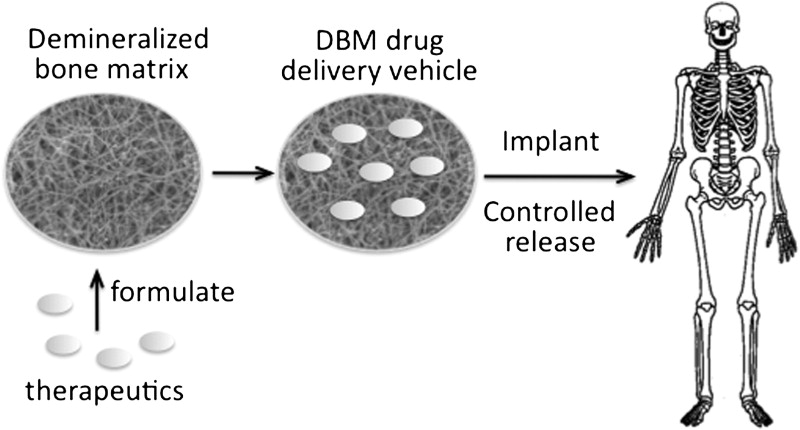
Demineralized Bone Matrix (DBM)

- Definition: Bone is processed to remove calcium, leaving behind proteins to stimulate bone healing.
- Advantages: Good scaffold for new bone growth, availability of growth-stimulating proteins.
- Disadvantages: Bone-forming cells are lacking, so they must be combined with other grafts.
DBM is a valuable scaffold that enhances bone formation when used with other bone graft materials.
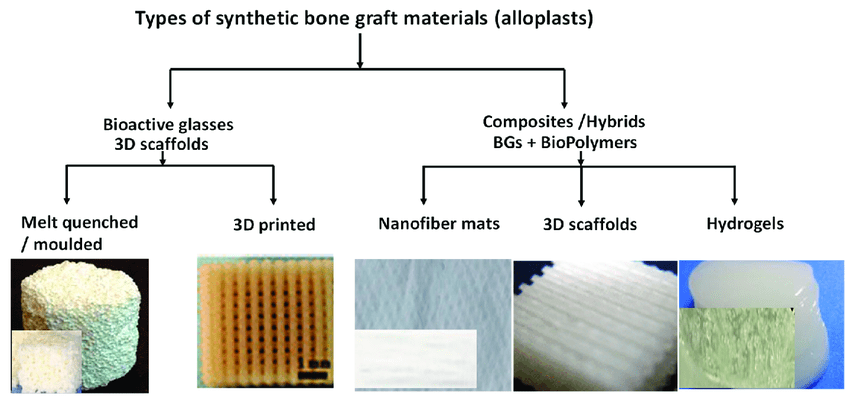
Synthetic Bone Grafts
- Definition: Man-made materials that mimic natural bone are typically made from calcium materials.
- Advantages: Unlimited supply, no disease transmission, customizable.
- Disadvantages: It may not integrate as well as natural bone, lacks cells and proteins, and requires combination with other graft types.
Synthetic grafts offer a reliable and scalable solution for bone grafting but need supplementation with biological materials to achieve optimal results.
Bone Marrow Aspirate
- Definition: Stem cells harvested from the patient’s bone marrow and combined with other graft materials.
- Advantages: Enhances healing potential, no disease transmission.
- Disadvantages: Additional procedure is required, and older adults have limited stem cell yield.
Bone marrow aspirate boosts the healing capabilities of other grafts, making it a valuable addition to the grafting process.
Biologics/Proteins
- Definition: Proteins such as Bone Morphogenetic Proteins (BMP) that stimulate bone growth.
- Advantages: Powerful bone-forming capabilities, reduces the need for autograft.
- Disadvantages: High cost, potential side effects, varying safety profiles.
Biologics like BMP offer a potent option for promoting bone growth, though carefully considering risks and benefits is essential.

Conclusion
Selecting the appropriate bone graft type for spinal fusion surgery is crucial for successful outcomes. This decision depends on various factors, including the patient’s condition, overall health, and specific surgical needs. Discussing these options with the surgical team ensures a tailored approach that maximizes the potential for effective spinal fusion and long-term pain relief.