Introduction:
Anterior Lumbar Interbody Fusion (ALIF) is a pivotal surgical intervention to rectify issues within the spine’s vertebrae.
Essentially likened to a welding process, spinal fusion entails the fusion of problematic or unstable vertebrae, fostering the formation of a cohesive, singular bone structure.
Purpose of Spinal Fusion:
The primary objective of spinal fusion is to address pain stemming from vertebral motion.
The procedure aims to alleviate discomfort by immobilising painful vertebrae, particularly in cases of arthritis, trauma, or fractures. Excessive spinal movement is mitigated through fusion, enhancing stability and reducing pain.
Focus on ALIF:
This article provides an in-depth exploration of anterior lumbar interbody fusion, concentrating solely on its surgical aspects.
While broader discussions on spinal fusion encompass various approaches, bone grafting techniques, complications, and rehabilitation, this piece exclusively delves into the intricacies of ALIF.
Approach:
During an anterior approach, organs and blood vessels are shifted aside to reveal the disk space.
While the posterior (back) approach is commonly used in spinal surgeries, there are situations where an anterior approach is preferred
This decision may be based on several factors:
- Avoidance of Multiple Surgeries: If a patient has undergone previous spinal surgeries using a posterior approach, opting for an anterior approach can prevent further interventions in the same area.
- Direct Access to the Intervertebral Disk: The anterior approach provides a more direct path to the intervertebral disk, enabling surgeons to precisely target the problem area.
- Ability to Adjust Spinal Alignment: Surgeons may choose an anterior approach to introduce additional lordosis (swayback) to the spine, improving overall spinal alignment.
- Potential for Faster Recovery: Some patients may experience quicker recovery times with an anterior approach than a posterior approach.
In contrast to the posterior approach, where nerves are moved, the anterior approach allows access to the spine without directly disturbing the nerves.
It does involve moving organs and blood vessels to the side. A vascular surgeon often assists the orthopaedic surgeon in opening and exposing the disk space.
Advancements in less invasive anterior fusion techniques have reduced muscle injury, further supporting faster recovery and improved patient outcomes.
Surgical Procedure:
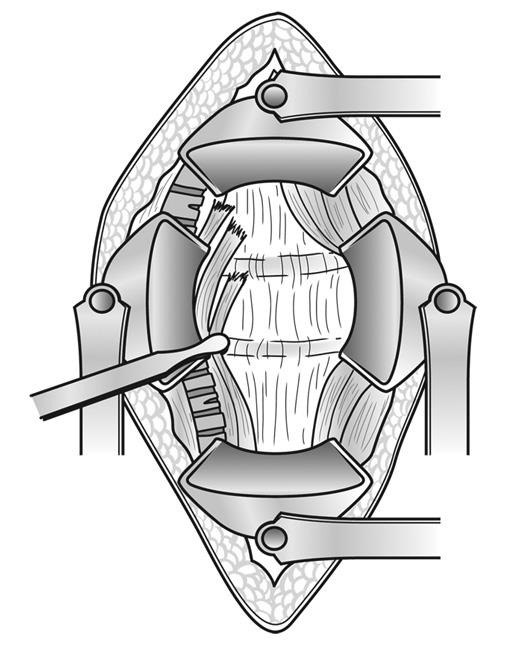
Initially, the surgeon, often assisted by a vascular specialist, will expose the targeted spine area.
Subsequently, the intervertebral disk is extracted from the disk space.
Once the disk space is cleared, the surgeon inserts a spacer between the adjacent vertebrae, commonly composed of metal, plastic, or bone. Typically containing bone graft material, this spacer facilitates bone healing and promotes the fusion process.
Stabilisation of the Spine:
Following the placement of the cage in the disk space, your surgeon may enhance spinal stability by utilising plates or screws to secure the cage in position.
This may be achieved through the same incision in some cases, while in others, additional screws may be inserted into the back of the spine through a separate incision (posterior approach).
Your surgeon will discuss with you beforehand which option is most suitable for your situation.
Incision Placement:
The orientation and location of your incision, whether horizontal or vertical, and positioned centrally or laterally, depend on your surgeon’s preference and comfort in accessing the spine.
Factors such as prior abdominal surgery may also influence this decision
Typically, the anterior procedure carries a lower complication rate compared to traditional spinal surgery. Potential drawbacks may include:
- Nerve damage, leading to weakness in foot movement
- Rare occurrences of bowel, bladder, or blood vessel injury (<0.1%)
- Incisional hernia, characterised by muscle protrusion
Consult your surgeon to find the approach that aligns best with your health requirements.
Recovery:
Following an ALIF procedure, patients typically remain in the hospital for one to three days, depending on pain management and mobility progress.
Patients are encouraged to stand and walk during the first day after surgery, often supported by a back brace provided by the surgeon to enhance comfort and safeguard the surgical fusion.
During the initial weeks after surgery, patients perform basic exercises like routine walking while avoiding bending, twisting, or lifting objects heavier than a gallon of milk.
Improvement in lower back pain and disability is commonly observed within weeks to months post-surgery for most ALIF patients.
Future Developments:
Advancements in technology and instrumentation may allow surgeons to perform ALIF surgery through smaller incisions in the spine’s front, potentially reducing pain and expediting recovery. However, regardless of the surgical approach, the biological fusion process of the spine remains consistent.
expandable cage technology permits surgeons to insert smaller devices that can be expanded to fit individual anatomy. This approach, facilitated by smaller incisions, may lower the risk of muscle and nerve damage.