If you often experience the sensation of “walking on a marble” or suffer from ongoing pain in the ball of your foot (forefoot), you might be dealing with a condition known as Morton’s neuroma.
While it is not a true tumor, this thickened tissue can cause varying degrees of pain or discomfort in the forefoot, potentially interfering with daily activities and physical mobility.. While it is not a true tumor, this thickened tissue can cause varying degrees of pain or discomfort in the forefoot, potentially interfering with daily activities and physical mobility.
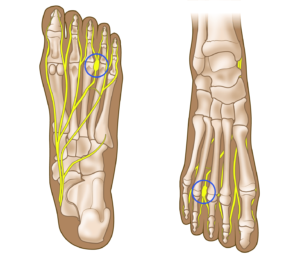
Anatomy of the Forefoot
The forefoot, or the front portion of the foot, consists of 14 toe bones (phalanges) and five metatarsal bones that connect the forefoot to the midfoot.
The spaces between the bases of the metatarsal bones, called web spaces, are integral to the forefoot’s structure. These web spaces are categorized as follows:
- First web space: Located between the big toe and second toe.
- Second web space: Found between the second and third toes.
- Third web space: Situated between the third and fourth toes.
- Fourth web space: Positioned between the fourth and little toes.
Sensory nerves in the forefoot, known as the medial and lateral plantar nerves, run along the sole of the foot and divide into branches near the toes. These branches, called common digital plantar nerves, provide sensation to parts of the toes and traverse the web spaces.
Within each web space, the rounded ends of the metatarsal bones are connected by structures known as transverse metatarsal ligaments. These ligaments support the common digital plantar nerves as they pass underneath, playing a crucial role in foot function.
 Plantar (underside) view of the foot showing the web spaces between the bases of the metatarsals, as well as the plantar nerves and transverse metatarsal ligaments.
Plantar (underside) view of the foot showing the web spaces between the bases of the metatarsals, as well as the plantar nerves and transverse metatarsal ligaments.