Superior and inferior pubic ramus fracture
Unstable Fracture
An unstable fracture occurs when there are two or more breaks in the pelvic ring, often accompanied by misalignment of the broken bone fragments (displacement). These fractures typically result from high-energy trauma, such as severe car accidents or significant falls.
Common patterns of unstable pelvic fractures include:
- Anterior-posterior compression fracture: Caused by force compressing the pelvis from front to back.
- Lateral compression fracture: Occurs when force is applied from the side of the pelvis.
- Vertical shear fracture: Results from upward force on one side of the pelvis, causing vertical displacement.
Classification of Pelvic Fractures
Pelvic fractures can be further categorized into two types based on skin integrity:
- Closed fractures: The skin remains intact, shielding the broken bones from external exposure.
- Open fractures: Bone fragments penetrate through the skin, creating an open wound. These fractures are particularly dangerous due to the heightened risk of infection in both the bone and surrounding tissues. Prompt medical intervention is essential to prevent complications.
Rephrased Section: Causes
High-Energy Trauma
High-energy impacts are a common cause of pelvic fractures, typically resulting from events such as:
- Motor vehicle or motorcycle accidents
- Crushing injuries
- Falls from significant heights (e.g., from a ladder)
The force of such incidents can cause life-threatening injuries, often necessitating surgical treatment to stabilize the pelvis and address associated trauma.
Bone Insufficiency
Weakened or insufficient bone strength, often due to conditions like osteoporosis, can also lead to pelvic fractures. These are most prevalent in older adults and may occur during minor events such as:
- Falls from standing height
- Routine activities, like getting out of a bathtub or descending stairs
Fractures caused by bone insufficiency are typically stable and involve a single pelvic bone, without compromising the structural integrity of the pelvic ring.
Other Causes
Less commonly, pelvic fractures may result from an avulsion fracture, where a small fragment of the ischium bone is pulled away at the attachment site of the hamstring muscles. This type of fracture is most common among young athletes still in their growth phase. Avulsion fractures generally do not compromise the pelvis’s stability or harm internal organs.
Rephrased Section: Symptoms
A pelvic fracture is typically accompanied by significant pain, which worsens with hip movement or attempts to walk. Many patients instinctively keep their hip or knee bent in a specific position to reduce discomfort. Other common symptoms include swelling and bruising around the hip region.
Doctor Examination
Emergency Stabilization
Patients with high-energy pelvic fractures are typically brought to an emergency room or urgent care center due to the severity of their symptoms. These injuries are often accompanied by trauma to other areas, such as the head, chest, abdomen, or legs. In cases of severe blood loss, patients may experience shock — a potentially fatal condition that can result in organ failure.
Treating high-energy pelvic fractures requires a multidisciplinary approach, involving specialists from various medical fields. In critical situations, doctors prioritize stabilizing the patient’s airway, breathing, and blood circulation before addressing the pelvic fracture and other injuries.
Physical Examination
During the examination, your doctor will:
- Thoroughly assess the pelvis, hips, and legs for signs of injury.
- Check for nerve damage by evaluating your ability to move your ankles and toes and feel sensations on the soles of your feet.
- Conduct a full-body assessment to identify any additional injuries.
Imaging Tests
- X-rays: These are the first-line diagnostic tool for all pelvic fractures, providing images of bone structures from multiple angles to assess the extent of displacement.
- Computed tomography (CT) scans: Due to the complexity of pelvic injuries, CT scans are frequently used. They offer detailed cross-sectional images, helping doctors understand the fracture pattern, identify related injuries, and plan surgical interventions if needed.
- Magnetic resonance imaging (MRI) scans: Although rare, MRI scans may be used to detect fractures that are not visible on X-rays or CT scans.

X-ray shows an unstable pelvic fracture with disruption of the pubis (arrow) and sacroiliac joint (arrowhead).
Treatment
The treatment approach for a pelvic fracture depends on several key factors, including:
- The specific fracture pattern.
- The degree of bone displacement (misalignment).
- The patient’s overall health and any additional injuries sustained during the trauma.
Nonsurgical Treatment
For stable fractures where bones remain in place or are only minimally displaced, nonsurgical treatment may be sufficient. This typically includes:
- Walking aids: To minimize weight-bearing on the affected leg, your doctor may recommend using crutches or a walker for up to three months, allowing time for the bones to heal. If both legs are injured, a wheelchair may be required temporarily to avoid putting pressure on either leg.
- Medications: Pain relievers may be prescribed to manage discomfort, alongside blood thinners (anticoagulants) to reduce the risk of blood clots forming in the legs or pelvic area.
Surgical Treatment
For unstable fractures, surgery is often necessary to stabilize the pelvis and promote proper healing. Common surgical procedures include:
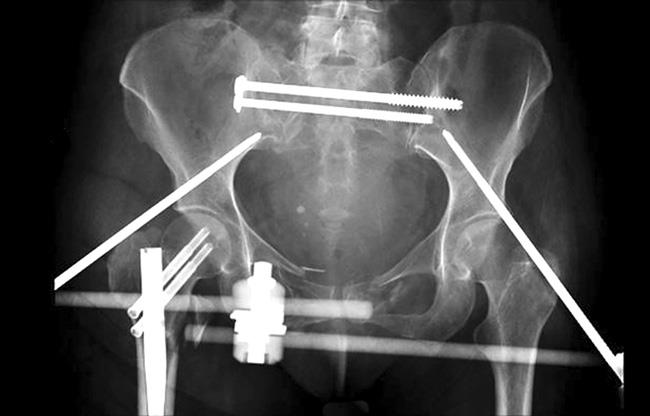
- External fixation: This technique involves the insertion of metal pins or screws into the pelvic bones through small incisions in the skin and muscles. These pins and screws extend outside the body and are connected to rigid carbon fiber bars, forming a stabilizing frame. The external fixator holds the bones in the correct position during healing.
In some cases, the external fixator is used as a temporary solution for stabilization until a more complex procedure can be performed. For patients unable to undergo lengthy surgeries, it may also serve as a primary treatment method.

In this X-ray, an external fixator has been used to stabilize the pelvis.
Open Reduction and Internal Fixation (ORIF)
In this surgical procedure, displaced bone fragments are carefully repositioned (reduced) to restore their normal alignment. Once aligned, the bones are stabilized using screws or metal plates, which are securely attached to the outer surface of the bone. This approach ensures the fracture heals correctly and restores the structural integrity of the pelvis.
 In this X-ray, plates and screws have been used to repair a fractured pelvis.
In this X-ray, plates and screws have been used to repair a fractured pelvis.
Complications
Like any surgical procedure, treatments for pelvic fractures carry certain risks. Before your surgery, your doctor will explain these risks in detail and implement measures to minimize the likelihood of complications.
Potential complications include:
- Wound healing issues: This may include delayed healing or infection at the surgical site.
- Nerve or blood vessel damage: Surgery in the pelvic region carries a risk of injuring nearby nerves or blood vessels.
- Blood clots: Clots may form in the veins of the legs or pelvis, posing a risk of further complications.
- Pulmonary embolism: A serious condition where a blood clot travels to the lungs, potentially causing life-threatening complications.
Your medical team will take all necessary precautions to reduce these risks and ensure a successful recovery.
Recovery
Pain Management
Experiencing pain after surgery is a normal part of the healing process. Your medical team will work to manage your discomfort, as effective pain relief can accelerate recovery.
Short-term pain relief may involve a combination of medications, including opioids, non-steroidal anti-inflammatory drugs (NSAIDs), and local anesthetics. This multi-modal approach helps reduce reliance on opioids, which can carry risks of dependency and addiction.
Opioids, while effective, must be used with caution. Follow your doctor’s instructions carefully and discontinue their use as soon as your pain improves. If your pain does not subside within a few days post-surgery, consult your doctor for further evaluation.
Early Movement
Your doctor will likely encourage early movement to facilitate recovery. Most patients start walking with weightbearing restrictions shortly after surgery. Simple foot and leg exercises may also be introduced to improve circulation and prevent complications.
Physical Therapy
Rehabilitation exercises play a vital role in recovery. Specific stretches will help you regain flexibility and restore range of motion in your hip, while strength-building exercises enhance muscle endurance to support daily activities.
Blood Clot Prevention
Limited mobility after surgery increases the risk of blood clots forming in the deep veins of your pelvis and legs. To mitigate this risk, your doctor may prescribe an anticoagulant (blood thinner) and encourage early movement as tolerated.
Weightbearing
Your doctor may recommend using crutches or a walker to minimize weightbearing during the initial healing phase. Full weightbearing is generally permitted around three months post-surgery, once the bones have healed. Some patients may require a cane or other walking aid for an extended period.
Outcomes
- Stable pelvic fractures: These typically heal well with minimal complications.
- Unstable pelvic fractures: Injuries from high-energy incidents, such as car accidents, can lead to severe complications like internal bleeding, organ damage, and infection. When treated successfully, these fractures also tend to heal effectively.
Post-injury, you may experience a temporary limp due to muscle damage around the pelvis, which can take up to a year to fully recover.
However, long-term issues such as pain, reduced mobility, and sexual dysfunction may arise from nerve or organ damage related to the fracture. These complications should be discussed with your doctor to explore appropriate treatment options.