Introduction :
An ankle fracture, also referred to as a broken ankle, happens when the bones within the ankle joint become fractured, varying from minor to severe cases requiring surgery and lengthy recovery.
While ankle fractures affect all ages, adults are more prone, ranking fourth in common fractures among them.
An ankle fracture profoundly impacts daily life, hindering activities like walking, driving, and work duties. Severe cases may immobilise the ankle for months, posing challenges in routine tasks.
Understanding causes, symptoms, and treatment options is crucial for managing ankle fractures effectively.
Swift symptom recognition and appropriate treatment are vital for favourable outcomes and for preventing complications.
This article delves into the causes of ankle fractures, identifying symptoms and available treatment choices.
Additionally, it offers insights into preventive measures to reduce fracture risk and recovery strategies for restoring mobility and confidence post-injury.
Anatomy
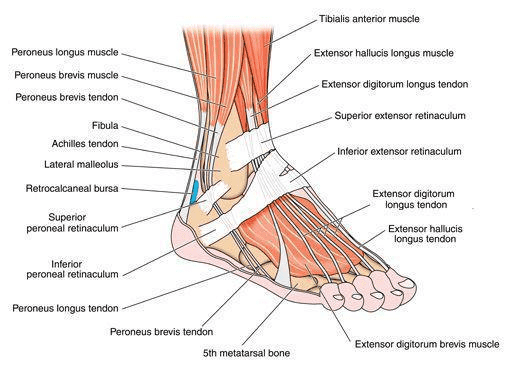
The ankle comprises specific parts of the tibia and fibula bones, including the medial malleolus, posterior malleolus, and lateral malleolus.
These structures stabilise the ankle joint and facilitate movements such as bending the foot up and down and side to side.
Ankle fractures are categorised based on the location of the bone breakage, such as a lateral malleolus fracture if the fibula’s end is fractured or a bimalleolar fracture if both the tibia and fibula are broken.
Ankle fractures involve two main joints: the ankle joint, where the tibia, fibula, and talus meet, and the syndesmosis joint, which connects the tibia and fibula with ligaments.
Description
Ankle fractures vary based on the displacement of bone fragments from their normal position:
- Nondisplaced fracture: In this type of ankle fracture, the bones remain properly aligned and do not require surgical intervention
- Displaced fracture: Here, the broken bone fragments are separated, potentially affecting one, two, or three ankle areas. Displaced fractures often necessitate surgical treatment, especially if the ankle joint is also dislocated.
- Open fracture occurs when fractured bones pierce through the skin, termed an open or compound fracture. It’s considered a medical emergency, requiring immediate surgical management to minimise infection risks associated with external contaminants infiltrating the fracture site.
Causes & Symtomes
Ankle fractures can result from various injuries, such as:
- Twisting, rotating, or rolling the ankle while walking or running
- Tripping or falling from a significant height, like falling off a ladder
- Impact during a car accident
Typical symptoms of an ankle fracture comprise:
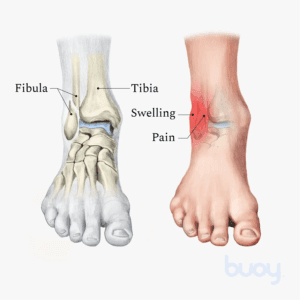
- Immediate and intense pain
- Swelling
- Bruising
- Tenderness upon touching
- Unable to put weight on your injured foot
- Deformity, especially if there’s a dislocation of the ankle joint
- Occasional numbness and coolness in the foot
Clinical examination
After discussing your medical history and the circumstances of the injury, your doctor will thoroughly examine your ankle, lower leg, and foot.
Imaging Procedures
If an ankle fracture is suspected, your physician may request one or more imaging tests to diagnose and assess the fracture.
Imaging tests :
X-rays:
Typically, X-rays are sufficient for diagnosing most ankle fractures. These images provide clear visuals of bone structures, indicating the location and displacement of fractures. Additionally, X-rays of the leg and foot may be taken to rule out any associated injuries.
In specific cases, your doctor might perform a stress X-ray by applying pressure to the ankle to assess the integrity of the syndesmosis, the area between the lower tibia and fibula.
Computed Tomography (CT) Scan:
A CT scan offers detailed cross-sectional images of the ankle, aiding in a more comprehensive evaluation of the injury’s extent, especially concerning the ankle joint.
Magnetic Resonance Imaging (MRI) Scan:
MRI scans produce highly detailed images of bone and soft tissue structures, such as ligaments. Due to their sensitivity, MRI scans are valuable for detecting ligament injuries and providing additional insights into the fracture’s nature.
Treatment
The treatment of ankle fractures varies depending on the type and severity of the injury.
Medial Malleolus Fracture
A medial malleolus fracture involves the lowest part of the tibia. Nonsurgical treatment, such as a short leg cast or walking boot, is typically sufficient for nondisplaced fractures.
Displaced fractures may require surgical intervention, often involving the placement of screws or plates to realign the bones.
Lateral Malleolus Fracture
Similar to medial malleolus fractures, lateral malleolus fractures can be managed nonsurgically with immobilisation devices like casts or walking boots.
Stable fractures allow weight-bearing on the ankle during the healing process, while unstable fractures may necessitate surgical repair using screws or plates.
Posterior Malleolus Fracture
Fractures at the back of the tibia, known as posterior malleolus fractures, may not always require surgery, especially if they are small.
larger or displaced fractures often require surgical fixation, typically involving screws to realign the bones.
Bimalleolar Fracture and Bimalleolar Equivalent Fracture
Fractures involving both the medial and lateral malleoli, termed bimalleolar fractures, usually require surgical repair due to their instability.
This may involve the use of plates and screws. Bimalleolar equivalent fractures, which involve ligament injuries and a single bone fracture, also often require surgical intervention.
Trimalleolar Fracture
Similar to bimalleolar fractures, trimalleolar fractures involve additional fractures at the back of the tibia. Surgical intervention may be necessary to stabilise the ankle joint and realign the bones.
Syndesmosis Injury
Injuries to the syndesmosis, the ligaments stabilising the ankle joint, may range from ligament sprains to ligament tears accompanied by fractures. While isolated ligament injuries may heal without surgery, complex cases may require surgical repair using screws or other fixation devices.
Surgical Repair of Syndesmosis Injury and Lateral Malleolus Fracture
Surgical intervention may be necessary to address combined injuries to the syndesmosis and lateral malleolus.
This typically involves repairing fractures and stabilising the syndesmosis with screws or other hardware.
Recovery
Recovery from ankle fractures can be variable, influenced by the severity of the injury. While healing typically takes a minimum of 6 weeks, additional time may be required for the complete restoration of ligaments and tendons.
Your physician will likely conduct regular X-rays to assess bone healing progress throughout the recovery process, usually within the initial six weeks.
Pain mangement
Pain management is an important aspect of your recovery journey. After surgery, you may experience discomfort as your body heals, but your medical team is here to help ease your pain.
Initially, pain medication will likely be administered intravenously to provide immediate relief, transitioning to oral medication as you recover.
There are various types of oral pain medications available, ranging from opioids to over-the-counter options like acetaminophen.
Your doctor may prescribe a combination of medications to manage your pain while minimising the need for opioids effectively.
It’s essential to follow your doctor’s instructions carefully when taking opioids, as they can be addictive.
Use them only as directed and taper off as your pain improves. Your comfort and well-being are our top priorities throughout your recovery process.
Rehabilitation
Rehabilitation is crucial in your recovery journey, regardless of your treatment.
Typically, rehabilitation begins once your fractures have healed and your cast or walking boot has been removed.
Your doctor will advise when it’s safe to start bearing weight on your ankle and may refer you to a physiotherapist to begin an exercise regimen.
It’s essential to adhere to your doctor’s guidance regarding weight-bearing activities. Putting weight on your injured ankle too soon can cause the fracture fragments to shift, hindering proper healing.
Your doctor may suggest wearing an ankle brace during sports activities for several months following the healing of your fracture. This extra support can help prevent re-injury and facilitate a smoother recovery process.
Complications Following Ankle Fracture
It’s common for patients to experience stiffness and swelling in the affected ankle for several months, even after the fracture has fully healed.
Rehabilitation is crucial in improving ankle motion and preventing stiffness, while elevating your leg can help alleviate swelling.
General complications may include malunion, where bones heal improperly, or nonunion, where bones fail to heal altogether.
Specific surgical complications may include infection, bleeding, damage to blood vessels, tendons, or nerves, and issues with the hardware used in ankle repair.
Certain factors like smoking, diabetes, or age can increase the risk of post-surgical complications.
Outcomes
Most individuals can resume normal activities within 3 to 4 months post-injury.
Resuming driving between 9 and 12 weeks for those affected on their right ankle, though some may continue to limp for several months.
Returning to sports activities may take longer, with complete recovery spanning up to 2 years.



