Introduction
Spinal injections are a critical component of pain management strategies, particularly for individuals suffering from chronic back pain, sciatica, herniated discs, and other spine-related conditions. These injections involve delivering medication directly into the spine to reduce inflammation and alleviate pain. This comprehensive guide aims to provide detailed information about spinal injections, including their types, indications, procedures, effectiveness, and more.
Types of Spinal Injections
2.1 Epidural Steroid Injections (ESI)
- Definition and Purpose: Epidural steroid injections are used to deliver steroids directly into the epidural space of the spine to reduce inflammation and pain.
- Procedure: The procedure involves the use of fluoroscopy (a type of X-ray) to guide the injection needle to the correct location.
- Benefits and Risks: The primary benefits include significant pain relief and reduced inflammation. Risks include infection, bleeding, and nerve damage.
2.2 Facet Joint Injections
- Definition and Purpose: These injections target the facet joints in the spine to relieve pain from arthritis or injury.
- Procedure: A steroid or anesthetic is injected directly into the facet joint using imaging guidance.
- Benefits and Risks: Benefits include pain relief and improved joint function. Risks may involve allergic reactions and temporary increase in pain.
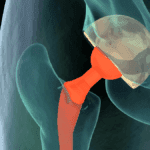
2.3 Sacroiliac Joint Injections
- Definition and Purpose: Aimed at alleviating pain in the sacroiliac joint, which connects the spine to the pelvis.
- Procedure: The injection is administered into the sacroiliac joint with the aid of imaging techniques.
- Benefits and Risks: Provides long-term pain relief. Risks include bleeding, infection, and temporary pain at the injection site.
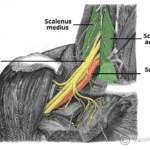
2.4 Medial Branch Blocks
- Definition and Purpose: These injections are used to block pain signals from the medial branch nerves that supply the facet joints.
- Procedure: Anesthetic is injected near the medial branch nerves using fluoroscopic guidance.
- Benefits and Risks: Helps in diagnosing and treating facet joint pain. Risks include localized pain and infection.
2.5 Selective Nerve Root Blocks (SNRB)
- Definition and Purpose: These injections target specific nerve roots to alleviate radicular pain (pain radiating from the spine to other parts of the body).
- Procedure: The injection is placed near the affected nerve root using fluoroscopy.
- Benefits and Risks: Effective for both diagnostic and therapeutic purposes. Risks include nerve damage and allergic reactions.
2.6 Trigger Point Injections
- Definition and Purpose: These injections treat painful muscle knots (trigger points) by injecting an anesthetic or steroid.
- Procedure: The medication is injected directly into the trigger point.
- Benefits and Risks: Provides pain relief and reduces muscle tension. Risks include infection and temporary pain.
Indications for Spinal Injections
3.1 Chronic Back Pain Chronic back pain is one of the most common reasons for spinal injections. These injections help in managing pain that persists for more than three months and does not respond to conservative treatments.
3.2 SciaticaSciatica is characterized by pain radiating from the lower back down to the legs. Spinal injections, particularly epidural steroid injections, can provide relief by reducing inflammation around the sciatic nerve.
3.3 Herniated Discs When a disc in the spine herniates, it can compress nearby nerves, causing pain and discomfort. Spinal injections can help reduce inflammation and relieve pain associated with herniated discs.
3.4 Spinal Stenosis Spinal stenosis involves the narrowing of the spinal canal, which can compress nerves and cause pain. Injections can reduce inflammation and alleviate symptoms associated with spinal stenosis.
3.5 Spondylolisthesis This condition involves the forward slippage of one vertebra over another, leading to nerve compression. Spinal injections can help manage pain and improve mobility in patients with spondylolisthesis.
3.6 Facet Joint ArthritisArthritis in the facet joints can cause significant pain and limit movement. Facet joint injections can reduce inflammation and provide pain relief for patients with facet joint arthritis.
Preparation for Spinal Injections
4.1 Pre-procedure Assessment A comprehensive medical evaluation is essential to determine if a patient is a suitable candidate for spinal injections. This assessment includes a review of medical history, physical examination, and imaging tests such as X-rays or MRI scans.
4.2 Medications to Avoid Patients may need to stop certain medications, particularly blood thinners, before the procedure to reduce the risk of bleeding. It is crucial to inform the healthcare provider about all medications being taken.
4.3 Fasting and Other Pre-procedure Instructions Patients are typically advised to fast for a few hours before the procedure. Other instructions may include avoiding smoking, arranging for transportation, and following specific guidelines provided by the healthcare provider.
The Procedure
5.1 Setting and Equipment Spinal injections are usually performed in a clinical setting such as a pain management clinic or hospital. The procedure requires specialized equipment, including needles, syringes, fluoroscopy or ultrasound machines, and medications.
5.2 Step-by-Step Procedure for Each Type of Injection
- Epidural Steroid Injections: The patient lies face down, and the injection site is cleaned and numbed. Using fluoroscopy, the needle is guided into the epidural space, and the steroid medication is injected.
- Facet Joint Injections: The patient lies on their stomach, and the injection site is prepared. A needle is inserted into the facet joint under imaging guidance, and the medication is delivered.
- Sacroiliac Joint Injections: The patient lies on their stomach, and the injection site is sterilized. A needle is guided into the sacroiliac joint using fluoroscopy, and the steroid is injected.
- Medial Branch Blocks: The patient lies on their stomach, and the area around the medial branch nerves is numbed. Using fluoroscopy, the needle is placed near the nerves, and the anesthetic is injected.
- Selective Nerve Root Blocks: The patient is positioned appropriately, and the injection site is prepared. The needle is guided to the nerve root using imaging, and the medication is injected.
- Trigger Point Injections: The patient may sit or lie down depending on the location of the trigger point. The area is numbed, and the needle is inserted directly into the trigger point to deliver the medication.
5.3 Role of Imaging Techniques (Fluoroscopy, Ultrasound) Imaging techniques such as fluoroscopy and ultrasound are crucial for guiding the needle to the precise location in the spine, ensuring accuracy, and minimizing the risk of complications. Fluoroscopy provides real-time X-ray images, while ultrasound offers detailed visualization of soft tissues and nerves.
Post-Procedure Care
6.1 Immediate Post-procedure Instructions After the injection, patients are typically observed for a short period to monitor for any immediate reactions or complications. Instructions may include rest, avoiding strenuous activities, and applying ice packs to reduce swelling.
6.2 Potential Side Effects and Complications Common side effects include temporary pain at the injection site, mild swelling, and bruising. Rare but serious complications can include infection, bleeding, nerve damage, and allergic reactions. Patients should be advised to seek medical attention if they experience severe pain, fever, or signs of infection.
6.3 Follow-up Care and Monitoring Follow-up appointments are essential to assess the effectiveness of the injection and to plan further treatment if needed. The healthcare provider may recommend additional injections, physical therapy, or other interventions based on the patient’s response to the initial injection.
Effectiveness of Spinal Injections
7.1 Evidence from Clinical Studies Numerous clinical studies have demonstrated the effectiveness of spinal injections in reducing pain and improving function in patients with various spinal conditions. These studies provide strong evidence supporting the use of spinal injections as part of a comprehensive pain management plan.
7.2 Patient Testimonials and Case Studies Patient testimonials and case studies highlight the real-world benefits of spinal injections. Many patients report significant pain relief, improved mobility, and enhanced quality of life following these procedures.
7.3 Comparison with Other Pain Management Techniques Spinal injections are often compared with other pain management techniques such as physical therapy, medications, and surgery. While injections may not be suitable for everyone, they offer a less invasive option with quicker recovery times compared to surgical interventions.
Risks and Complications
8.1 Common Risks
- Infection: There is a risk of infection at the injection site, which can be minimized by following proper sterile techniques.
- Bleeding: Patients on blood thinners or with bleeding disorders may be at higher risk.
- Temporary Pain: Some patients may experience temporary pain or discomfort at the injection site.
8.2 Rare but Serious Complications
- Nerve Damage: Incorrect needle placement can result in nerve damage, leading to pain, weakness, or numbness.
- Paralysis: Although extremely rare, there is a risk of paralysis if the spinal cord or major nerves are affected.
- Severe Allergic Reactions: Allergic reactions to the medications used in the injection can occur, requiring immediate medical attention.
8.3 How to Minimize RisksTo minimize the risks, it is essential to:
- Conduct a thorough pre-procedure assessment.
- Use imaging guidance for accurate needle placement.
- Follow sterile techniques to prevent infections.
- Monitor patients closely during and after the procedure.
Advances in Spinal Injection Techniques
9.1 New Technologies and Methods Advancements in technology have led to the development of new spinal injection techniques, including the use of robotic assistance, augmented reality, and computer-guided navigation systems. These innovations aim to enhance precision and improve patient outcomes.
9.2 Role of Regenerative Medicine (PRP, Stem Cells) Regenerative medicine, including platelet-rich plasma (PRP) and stem cell injections, is emerging as a promising area in spinal care. These treatments promote tissue healing and regeneration, offering potential benefits for patients with degenerative spinal conditions.
9.3 Future Directions in Spinal Injections The future of spinal injections lies in the continued development of less invasive techniques, improved imaging technologies, and personalized treatment approaches. Ongoing research and clinical trials will further expand the understanding and application of these advanced methods.
Frequently Asked Questions (FAQs)
10.1 What Conditions Can Spinal Injections Treat? Spinal injections can treat various conditions, including chronic back pain, sciatica, herniated discs, spinal stenosis, spondylolisthesis, and facet joint arthritis.
10.2 How Long Do the Effects of Spinal Injections Last? The duration of pain relief varies among individuals and depends on the type of injection and underlying condition. Some patients experience relief for several weeks to months, while others may require repeated injections.
10.3 Are Spinal Injections Painful? Patients may experience mild discomfort during the procedure, but local anesthesia is typically used to minimize pain. Post-procedure pain is usually mild and temporary.
10.4 How Often Can I Receive Spinal Injections? The frequency of spinal injections depends on the patient’s condition and response to treatment. Healthcare providers generally limit the number of injections to avoid potential side effects from repeated steroid use.
10.5 What Should I Expect During Recovery? Recovery from spinal injections is typically quick, with most patients resuming normal activities within a few days. Patients should follow their healthcare provider’s instructions, which may include rest, limited physical activity, and follow-up appointments.
Conclusion
11.1 Summary of Key Points Spinal injections offer a valuable option for managing various spinal conditions. They provide significant pain relief, reduce inflammation, and improve function with minimal invasiveness.
11.2 Final Thoughts on Spinal Injections in Pain Management Spinal injections play a crucial role in pain management, offering a less invasive alternative to surgery. They are effective for many patients and can be part of a comprehensive treatment plan.
11.3 Encouragement to Consult with a Healthcare Provider for Personalized Advice It is essential for patients to consult with a healthcare provider to determine the most appropriate treatment for their condition. Personalized medical advice ensures the best possible outcomes.