Definition
Lateral epicondylitis, commonly known as tennis elbow, involves tendinosis at the origin of the common wrist extensors. A more accurate term is lateral elbow tendinopathy, reflecting the condition’s degenerative nature.
Anatomy
The common extensor origin is located on the lateral epicondyle of the humerus. This origin includes the extensor carpi radialis brevis (ECRB), extensor digitorumcommunis (EDC), extensor digitiminimi, and extensor carpi ulnaris. The ECRB is most commonly affected, followed by the EDC, with their tendons becoming confluent at their origin.
Pathogenesis
Lateral epicondylitis results from repetitive microtrauma, leading to an incomplete reparative response and chronic tendinosis. This condition is often associated with activities involving repetitive forceful gripping, lifting, pulling, twisting, and pushing objects. Recent studies have found a high prevalence of concurrent radiocapitellar cartilage lesions in patients with lateral epicondylitis, observed during arthroscopic examinations.
Natural History
Lateral epicondylitis is generally a self-limiting condition, resolving in over 80% of patients within one year. Most patients improve with nonoperative treatments such as anti-inflammatory medications, orthotics, ultrasound, physical or occupational therapy, and injections. Fewer than 10% of patients require surgical intervention.
Patient History and Physical Findings
Phases of Lateral Epicondylitis:
- Acute Phase: Pain or ache in the lateral elbow occurs with activities and typically resolves with rest, ice, or anti-inflammatory medication.
- Intermediate Phase: Pain or ache occurs with activity and at rest, which may not resolve without prolonged activity restriction.
- Chronic Phase: Pain or ache occurs during sleep and is unresponsive to rest, medication, and injections.
Examination Methods:
- Palpation: Tenderness over the lateral epicondyle is a universal finding.
- Passive Stretch Test: Elbow in full extension, wrist flexed, and forearm pronated. Pain indicates a positive test.
- Mill Test: Elbow flexed, forearm slightly pronated, wrist slightly dorsiflexed. The patient actively supinates against resistance. Pain indicates a positive test.
- Thompson Test: Elbow extended, wrist in slight dorsiflexion, making a fist. The patient dorsiflexes against resistance. Pain indicates a positive test.
Imaging and Other Diagnostic Studies
- Plain Radiographs: May show calcifications at the extensor origin.
- Magnetic Resonance Imaging (MRI):
- Increased intratendon signal is reliably demonstrated on T2-weighted sequences.
- Increased intratendon signal or tendon thickening may be seen on T1-weighted sequences.
- Some patients may show increased T2 signal in the lateral epicondyle or anconeusedema.
- Lateral collateral ligament tears may be over-interpreted on MRI reports, requiring confirmation through history and clinical examinations.
Differential Diagnosis
- Synovial plica
- Radial tunnel syndrome
- Cervical radiculopathy
- Osteochondritisdissecans
- Intra-articular loose bodies
- Lateral collateral ligament injury
- Posterolateral rotatory instability
Nonoperative Management
Initial treatment includes activity modification, nonsteroidal anti-inflammatory drugs (NSAIDs), physical or occupational therapy, bracing, and possibly corticosteroid injections. These methods aim to reduce inflammation and promote healing.
Surgical Management
Surgery is considered for patients who do not respond to nonoperative treatment after 6 to 12 months. Both open and arthroscopic approaches aim to debride the degenerative tissue and stimulate healing.
Preoperative Planning
- Patient Assessment: Comprehensive history and physical examination to confirm the diagnosis and rule out other pathologies.
- Imaging: Review of MRI and radiographs to assess the extent of tendinosis and rule out associated conditions.
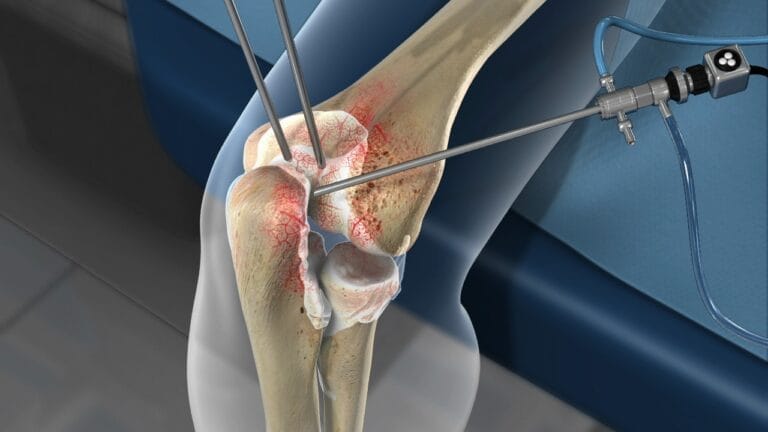
Surgical Techniques
- Open Surgery: Involves a small incision over the lateral epicondyle, debridement of the degenerative tissue, and possible repair of the extensor origin.
- Arthroscopic Surgery: Minimally invasive technique using small incisions and a camera to visualize and debride the affected tendons.
Postoperative Care
- Rehabilitation: Early mobilisation to prevent stiffness and a structured physical therapy program to restore strength and function.
- Activity Modification: Gradual return to activities, avoiding repetitive stress on the extensor tendons.
Lateral epicondylitis is a common condition that can be effectively managed with nonoperative and operative treatments. Accurate diagnosis, appropriate treatment planning, and adherence to rehabilitation protocols are essential for optimal patient outcomes.