Overview:
Acromioclavicular (AC) joint injuries are common among young men aged 20 to 30, particularly those involved in sports. These injuries range from simple ligament sprains to more severe displacements of the collarbone. Treatment options vary, and the best method depends on the specific injury and its severity.
What is the AC Joint?
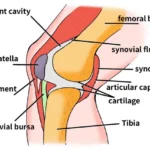
The AC joint is where the collarbone (clavicle) meets the highest point of the shoulder blade (acromion). It is essential for shoulder movement and stability.
Causes of AC Joint Injuries:
- Direct Impact: A direct hit to the shoulder, often seen in contact sports like football or rugby.
- Falls: Falling onto an outstretched hand or directly onto the shoulder can cause an AC joint injury.
Symptoms of AC Joint Injuries:
- Pain: Sharp pain at the top of the shoulder.
- Swelling and Bruising: Visible swelling and bruising around the joint.
- Deformity: A noticeable bump or displacement at the AC joint.
- Limited Movement: Difficulty or pain when moving the arm and shoulder.
Diagnosing AC Joint Injuries:
- Physical Examination: The doctor will check for pain, swelling, and deformity.
- Imaging:
- X-rays: Special views like the Zanca view are used to see the AC joint clearly.
- CT and MRI: These can provide additional details, especially for assessing soft tissue injuries.
Types of AC Joint Injuries:
- Rockwood Classification: A commonly used system that categorizes injuries based on the extent of ligament damage and displacement.
- ISAKOS Classification: A more refined approach that helps in making better treatment decisions.
Treatment Options:
- Non-Surgical Management:
- Suitable for mild injuries (Grade I and II) and some moderate injuries (Grade III).
- Pain Relief: Medications to manage pain.
- Sling Immobilization: To support the shoulder and allow healing.
- Physiotherapy: Exercises to restore shoulder movement and strength.
- Surgical Management:
- Needed for more severe injuries (Grade IV-VI) or unstable moderate injuries (Grade IIIB).
- LARS LigamentReconstruction: A technique to stabilsze the joint using synthetic ligaments.
- Biological Graft Reconstruction: Using tendons from the patient or a donor.
- Hook Plate Fixation: A metal plate to hold the bones in place, later removed in a second surgery.
Post-Operative Rehabilitation:
- Early Exercises: Gentle movements to prevent stiffness.
- Gradual Progression: Moving to more active exercises and strengthening routines as healing progresses.
Possible Complications:
- Infection: Risk of infection after surgery.
- Implant Failure: Issues with the surgical hardware.
- Stiffness and Arthritis: Long-term joint issues.
Lessons Learned:
- Accurate diagnosis and imaging are crucial for effective treatment.
- Conservative management works well for less severe injuries.
- Surgical options are available for more severe or unstable injuries.
- Early rehabilitation and physiotherapy are vital for recovery.
- Understanding different surgical techniques and potential complications helps tailor treatment to individual needs.