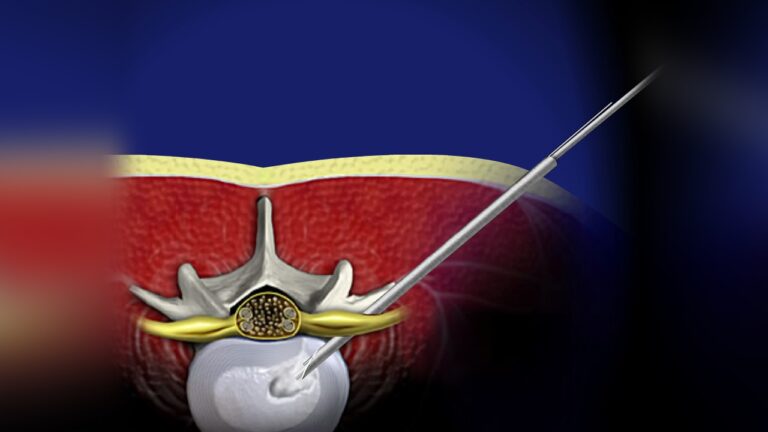
Overview of Endoscopic Diskectomy
Endoscopic spine surgery is an advanced, minimally invasive procedure used to treat herniated disks in the lower back. This technique involves the use of an endoscope—a thin, flexible tube equipped with a camera and light source—that allows surgeons to access and visualize the spine through small incisions.
With its numerous potential benefits, endoscopic diskectomy has become a popular and effective alternative to traditional open spine surgery and microdiskectomy, offering faster recovery and reduced tissue damage.
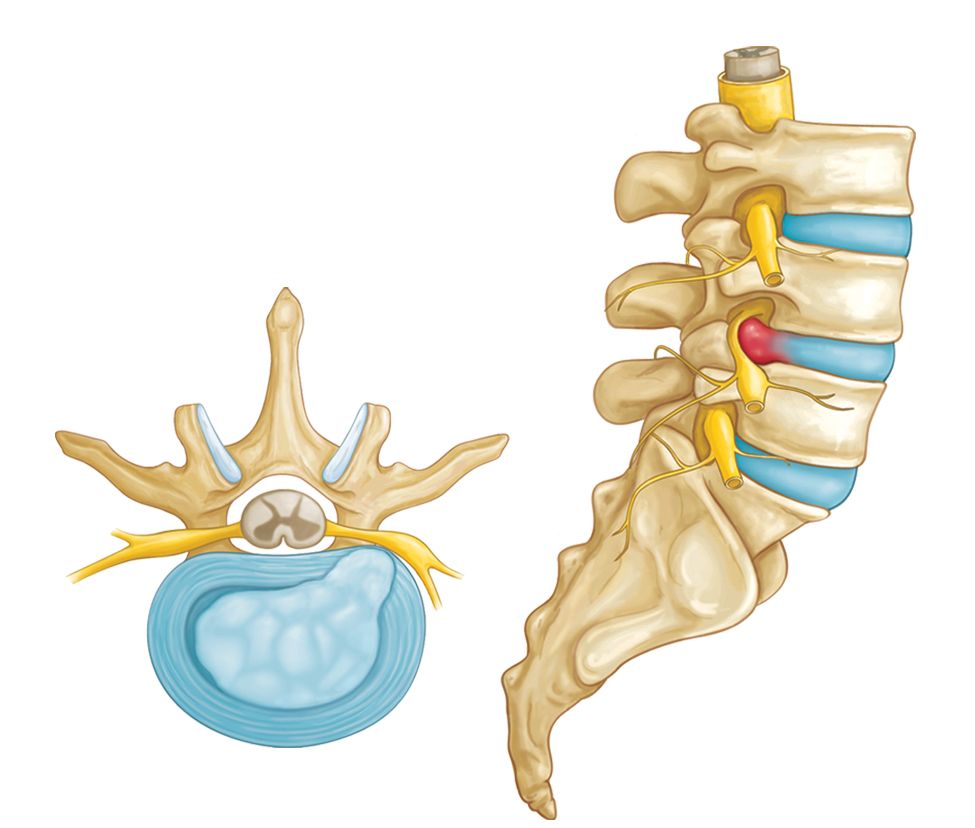
Description of a Herniated Disk
A disk herniates when its jelly-like nucleus begins to push against the outer ring due to wear and tear or a sudden injury. This pressure on the outer ring can cause lower back pain.
If the pressure persists, the nucleus may fully push through the outer ring or cause it to bulge. This can exert pressure on the spinal cord and nerve roots, leading to both mechanical compression and chemical irritation from the disk material.
When the nerve roots become inflamed or compressed, symptoms such as:
- Pain,
- Numbness, and
- Weakness in one or both legs may occur—a condition known as sciatica.
Endoscopic diskectomy aims to relieve these symptoms by removing the herniated portion of the disk while preserving surrounding tissues.