Rephrased Paragraph:
A thumb fracture can lead to significant challenges, as impaired thumb function impacts your ability to grip and handle objects effectively. Certain fractures in the thumb are particularly concerning, as they may raise the likelihood of developing arthritis as you age.
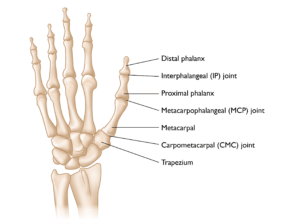
Anatomy
The thumb’s functionality relies on multiple bones working together in coordination. The bone beneath the nail, forming the tip of the thumb, is known as the distal phalanx. Just below it lies the proximal phalanx, which connects to the distal phalanx through the interphalangeal (IP) joint, enabling you to bend the tip of your thumb.
Moving down, the thumb is linked to the hand via the metacarpophalangeal (MCP) joint, situated between the proximal phalanx and the first metacarpal bone in the hand. The first metacarpal then attaches to the wrist at the carpometacarpal (CMC) joint, positioned between the metacarpal and a wrist bone called the trapezium.
The thumb also features a webbed area between it and the index finger, allowing for the outward motion needed to grasp objects. Key ligaments at each thumb joint support mobility while maintaining joint stability, preventing dislocation:
- The flexor pollicis longus (FPL), running along the palm side of the thumb, enables thumb flexion.
- The extensor pollicis longus (EPL), located on the back side of the thumb, facilitates thumb extension.
In addition, other tendons and muscles contribute to the thumb’s wide range of motion. Sensory nerves provide touch sensation, and blood vessels supply circulation essential for thumb function.

Description
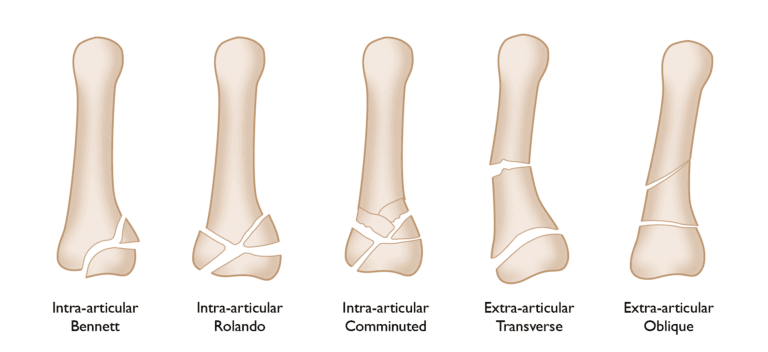
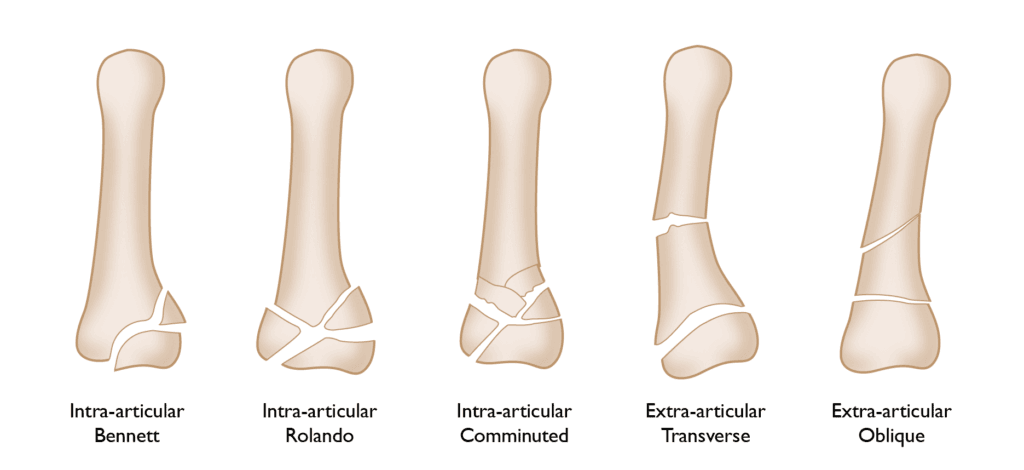
All thumb bones are vulnerable to fractures, with those impacting joints often posing the greatest challenges. Fractures involving joint areas generally require more complex treatment and carry a higher risk for adverse outcomes.
The most frequent thumb fractures affect the base of the first metacarpal, impacting the CMC joint where the thumb connects to the wrist:
- A Bennett fracture involves a clean break at the base of the thumb metacarpal, with a distinct fragment of bone separating.
- A Rolando fracture is similar but more complex, as it shatters the bone into multiple pieces.
Fractures along the long portion of the thumb’s metacarpal, known as the metacarpal shaft, are also possible and are often simpler to manage than those affecting the joint.
The distal and proximal phalanges are likewise susceptible to fractures. Similar to the metacarpal, these bones can fracture either near or into a joint or along their shafts.
In some cases, thumb fractures can destabilize joints if they involve crucial ligaments that keep the joints aligned. These are often avulsion injuries, where a ligament is forced to detach from its connection point, sometimes pulling a fragment of bone with it. Such injuries resemble ligament damage and are usually treated accordingly.

Causes
Thumb fractures typically occur due to direct trauma, such as from a fall or a hard impact to the hand. These fractures can also result from sports incidents, for instance, when a ball forcefully pulls the thumb backward. Some thumb fractures occur indirectly through twisting motions or strong muscle contractions, often seen in activities like wrestling, hockey, football, and skiing. Individuals with a history of bone diseases or calcium deficiencies face a higher risk of experiencing thumb fractures.
Preventative measures, such as protective taping, padding, and specialized equipment, can help reduce the likelihood of a thumb fracture. Strengthening hand muscles through regular exercise and ensuring a balanced diet with adequate calcium are additional steps that may offer protective benefits.
Symptoms
Common symptoms of a thumb fracture include:
- Intense pain at the fracture site
- Swelling around the thumb
- Limited or inability to move the thumb
- Extreme tenderness when touching the thumb
- A misshapen or deformed appearance of the thumb
- Numbness or a feeling of coldness in the thumb
- Joint instability within the thumb
Doctor Examination
If a thumb injury occurs and a fracture is suspected, it is essential to consult a doctor promptly. Delaying treatment may complicate bone alignment and potentially impact recovery. Using a padded splint to stabilize the thumb and prevent further misalignment is often recommended before receiving complete medical care.
During the examination, the physician will review the injury and your medical history, often supported by X-rays. They will also:
- Assess the tendons and nerves to ensure no additional injuries are present
- Examine surrounding digits and the rest of the hand for related injuries
- Check the thumb’s ligaments to confirm strength and absence of injury
Treatment Options
Nonsurgical Treatment
For thumb fractures where the bone fragments have not significantly shifted, or if the break is along the middle (shaft) of the bone, nonsurgical treatment may be effective. In such cases, your surgeon might use a specialized cast, known as a spica cast, to keep the bone fragments stable during healing. Typically, this cast is worn for 4 to 6 weeks, with regular X-rays taken to ensure the bone remains correctly aligned.

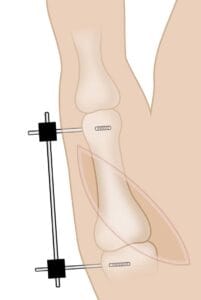
A fracture of the thumb can be held in proper alignment using external fixation.
Reproduced with permission from Soyer AD: Fractures of the Base of the First Metacarpal: Current Treatment Options. J Am Acad Orthop Surg 1999;7:403-412.
Surgical Treatment
Surgical intervention may be required depending on the fracture’s location, bone alignment, and the extent of movement between fragments. Various fixation techniques may be used to realign and stabilize the broken pieces for healing.
- Internal fixation uses devices like wires, pins, plates, and screws to hold the fragments in place within the body.
- External fixation involves inserting pins into the bone, which are secured to an external device for stability.
Each treatment option has its advantages and potential drawbacks. Your surgeon will discuss the most suitable approach for your specific fracture. After surgery, a cast or splint may be required for an additional 2 to 6 weeks. Once the cast is removed, hand therapy is often recommended to restore mobility in the thumb, as full recovery may take up to 3 months or more, depending on the injury’s severity.