Neurofibromatosis is a genetic disorder that affects the development and growth of nerve cell tissues, causing tumours known as neurofibromas to grow on nerves. These tumours are usually benign (noncancerous) and can appear on nerves within the body and on and under the skin. This disorder can impact various systems in the body, including the skin, skeleton, and brain. While neurofibromatosis often presents symptoms at birth or during childhood, the severity can vary widely among individuals.
Types of Neurofibromatosis
There are three main types of neurofibromatosis, each with distinct characteristics and symptoms.
1. Neurofibromatosis Type 1 (NF1)
Neurofibromatosis Type 1, also known as von Recklinghausen disease, is the most common form, occurring in approximately 1 in 3,000 to 4,000 births. NF1 primarily affects the peripheral nervous system.
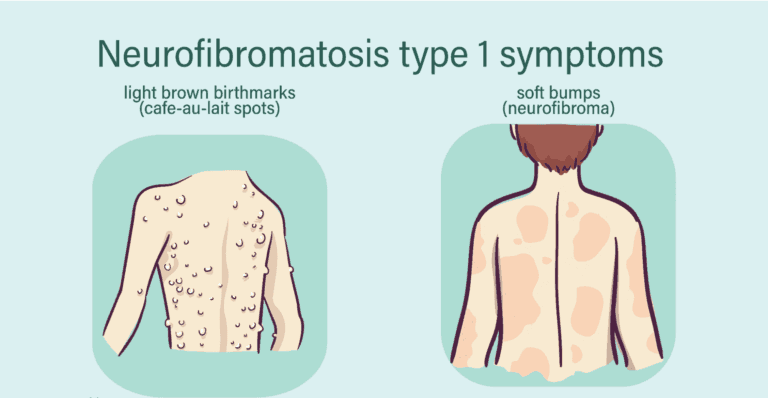
Symptoms of NF1:
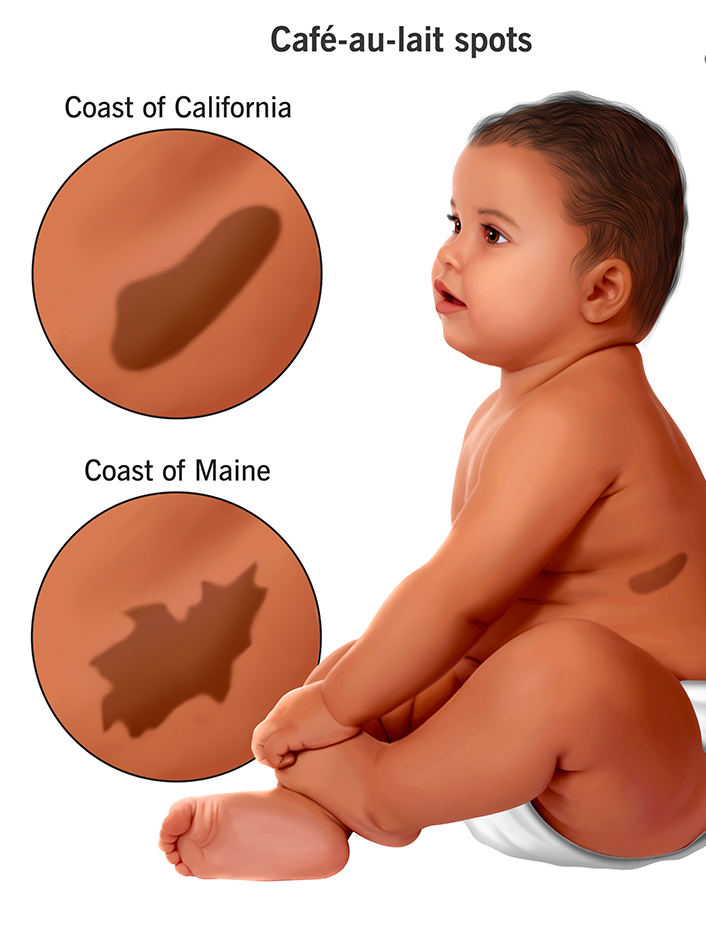
- Café-au-lait Spots:
- These light brown birthmarks are a hallmark of NF1. Six or more spots more prominent than 5mm in children and 15mm in adolescents often indicate the condition.
- Freckling:
Freckling in the armpit and groyne areas (axillary and inguinal freckling) is expected.
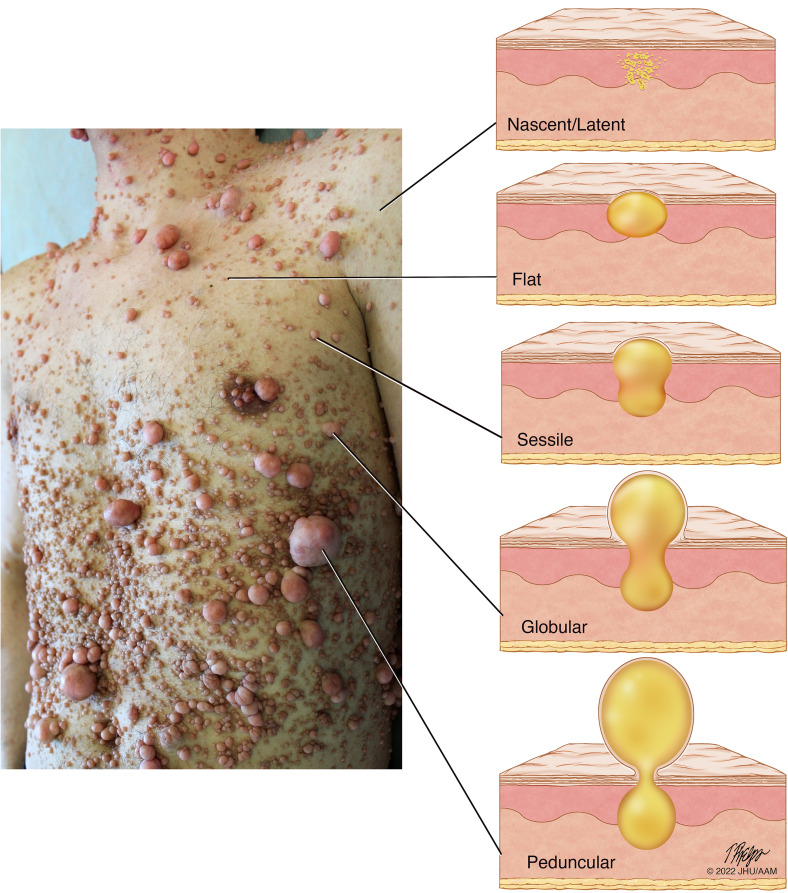
- Neurofibromas:
Small, painless, and slow-growing tumours that may form nodules on the skin or masses deep within the body. They can appear at any age but often manifest around adolescence.
- Optic Gliomas: Tumours on the nerves of the eyes that can affect vision.
- Plexiform Neurofibromas: Larger tumours involving multiple nerves, potentially causing disfigurement, pain, or weakness in the arms or legs.
Other Complications:
- Lisch Nodules: Small brown tumours on the iris that do not affect vision.
- Learning Disabilities:Many children with NF1 have learning disabilities, delayed development, speech problems, short stature, an oversized head (macrocephaly), and an increased risk of cancer.
- Orthopaedic Issues: These include scoliosis (a sideways curve of the spine) and congenital pseudarthrosis of the tibia (abnormal growth of the shinbone leading to bowing and fractures).
2. Neurofibromatosis Type 2 (NF2)
Neurofibromatosis Type 2 is less common, occurring in about 1 in 25,000 to 40,000 births. NF2 primarily affects the central nervous system, leading to tumour brain and spinal cord tumours.
Symptoms of NF2:
- Hearing Loss: Often the first symptom, beginning in the teens or early 20s, due to tumours on the auditory nerves.
- Other Symptoms: Ringing in the ears, headaches, facial pain or numbness, and balance issues.
3. Schwannomatosis
Schwannomatosis is the rarest form of neurofibromatosis and does not typically affect the musculoskeletal system. It is characterised by painful tumours called schwannomas, which grow on nerves. Mutations in the SMARCB1 or LZTR1 genes cause this condition.
Causes of Neurofibromatosis
Genetic mutations cause neurofibromatosis. Each type of neurofibromatosis is linked to a specific gene:
- NF1: Caused by mutations in the NF1 gene, which provides instructions for making a neurofibromin protein. About 50% of NF1 cases are inherited in an autosomal dominant manner, meaning one copy of the altered gene is sufficient to cause the disorder. The remaining cases result from spontaneous mutations.
- NF2: Caused by mutations in the NF2 gene, which acts as a tumour suppressor. Similar to NF1, about half of NF2 cases are inherited, while the other half result from spontaneous mutations.
Diagnosing Neurofibromatosis
Diagnosis involves a thorough medical history, physical examination, and various tests:
- Medical History and Physical Examination: The doctor will discuss symptoms and their onset and examine for changes in skin appearance, tumours, or bone abnormalities. Family members may also be reviewed to look for signs of neurofibromatosis.
- X-rays: Used to detect skeletal deformities.
- Magnetic Resonance Imaging (MRI): Provides detailed images of soft tissues to detect tumours early.
- Biopsy: A sample of tumour tissue may be examined under a microscope to check for cancer cells.
Managing Neurofibromatosis
While there is no cure for neurofibromatosis, treatment focuses on managing symptoms and preventing complications. This often involves a team of medical specialists, including orthopaedic surgeons, neurologists, dermatologists, and radiologists.
General Guidelines for Treatment:
- Regular Medical Evaluations: Children with neurofibromatosis need regular check-ups to monitor growth blood pressure, and check for new symptoms.
- Early Detection: Screening tools and regular eye exams help detect optic nerve gliomas before they cause significant vision loss.
- Annual Evaluations: Adults with neurofibromatosis often require yearly check-ups to monitor their nervous system and hearing.
- Multidisciplinary Clinics: Some patients benefit from comprehensive evaluations at specialised neurofibromatosis clinics.
Treatment of Tumours:
- Observation: Most tumours do not need immediate treatment but should be monitored for changes.
- Surgery: Tumours that are painful, disfiguring, or rapidly growing may need to be surgically removed.
- Radiation and Chemotherapy: These treatments can shrink tumours and destroy cancer cells if they become malignant.
Orthopaedic Treatment:
- Scoliosis: Mild curves may be managed with bracing, while severe cases may require spinal fusion surgery.
- Congenital Pseudarthrosis of the Tibia: Special braces can prevent fractures. Surgery may be needed to align and stabilise the bone.
Living with Neurofibromatosis
Living with neurofibromatosis can be challenging, both physically and emotionally. The condition often causes visible differences that can lead to isolation and self-consciousness. Emotional support is crucial for both patients and their families.
Support and Counseling:
- Family Counselling: Helps families cope with the emotional impact of the diagnosis.
- Genetic Counselling: Provides information about the risk of passing the condition to children.
- Support Groups: Offer emotional support and practical advice from others facing similar challenges.
Conclusion
Neurofibromatosis is a complex genetic disorder with a wide range of symptoms and complications. Understanding the types, causes, symptoms, and treatment options is crucial for managing the condition effectively. Regular monitoring, early intervention, and a comprehensive care plan involving multiple specialists can help improve the quality of life for those affected by neurofibromatosis.
By staying informed and proactive, patients and their families can navigate the challenges of neurofibromatosis and seek the best possible care. If you or a loved one has been diagnosed with neurofibromatosis, consult with healthcare professionals for a tailored treatment plan and support resources.