Introduction to Peroneal Tendon Subluxation
The peroneal tendons belong to two muscles located along the outer edge of the lower leg. These tendons pass through a fibrous tunnel positioned behind the lateral malleolus (the outer ankle bone). When the structures that form or support this tunnel are damaged or injured, the peroneal tendons can slip out of place, leading to a condition known as peroneal tendon subluxation.
This guide will help you understand:
- How peroneal tendon subluxation occurs
- How the condition is diagnosed by doctors
- Available treatment options for managing this problem
Anatomy: What Part of the Ankle is Involved?
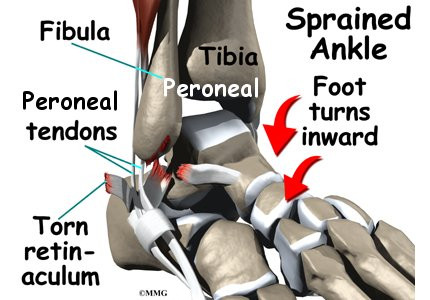
The primary muscles supporting the lateral (outer) part of the ankle are the peroneals. These two muscles and their tendons run along the outer side of the lower leg bone, the fibula, and cross behind the lateral malleolus (the outer ankle bone).
The tendons of the peroneal muscles pass through a groove located behind the lateral malleolus. This groove is covered by a sheath, which forms a protective tunnel around the tendons. The sheath’s surface is reinforced by a ligament band called the retinaculum, which helps secure the tendons in place.
When the peroneal muscles contract, their tendons glide smoothly through the groove, functioning like a pulley. This action allows the foot to move downward (plantarflexion) and outward (eversion).

Causes: Why Does Peroneal Tendon Subluxation Occur?
Tendons connect muscles to bones, transmitting tension created by muscle contractions to move the bones. Many tendons are secured in place by supportive connective tissues such as ligaments or the retinaculum. When these supportive tissues are damaged, tendons can slip out of their normal position, a condition called subluxation. If the tendon returns to its proper place, it is said to relocate. However, if the tendon is forcefully displaced and cannot relocate, it is considered dislocated.
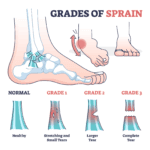
1. Ankle Sprains
The most common cause of peroneal tendon subluxation is an ankle sprain. During a typical inversion ankle sprain, the foot rolls inward, stretching the peroneal tendons and potentially tearing the retinaculum. This tear allows the tendons to move out of their groove and then snap back into place. Initially, the focus of treatment may be on damaged ankle ligaments, leaving injuries to the retinaculum undiagnosed. Over time, this snapping motion may become chronic and persistent, even if it was not initially recognized as part of the original ankle sprain.
2. Acute Dislocation
Acute dislocation of the peroneal tendons is rare but can occur during sports activities that force the foot upward and inward, such as skiing, ice skating, or soccer. In these scenarios, the peroneal muscles contract violently to stabilize the ankle, which can tear the retinaculum and allow the tendons to slip out of their groove.
3. Anatomical Differences
Certain anatomical variations may predispose individuals to peroneal tendon subluxations, even without a history of injury. These include:
- A shallow groove behind the lateral malleolus.
- A small or absent ridge that normally deepens the groove.
- A loose retinaculum, unable to keep the tendons securely in place.
Patients with these anatomical differences may experience persistent snapping of the peroneal tendons without a clear injury to explain the condition.
Symptoms: What Does Peroneal Tendon Subluxation Feel Like?
Patients commonly report a popping or snapping sensation along the outer edge of the ankle. In some cases, the tendons can visibly slip out of place around the lower tip of the fibula. Additional symptoms include:
- Pain and tenderness along the tendons
- Swelling just behind the bottom edge of the fibula
Diagnosis: How Is Peroneal Tendon Subluxation Identified?
Diagnosis begins with a thorough physical examination of the ankle. During the exam, your doctor will move the ankle into various positions to observe when the tendons snap out of place and whether they relocate. One specific test involves pressing down on the ankle while you lift and turn your foot outward. The doctor feels behind the fibula during this maneuver to detect if the tendons are popping out of their groove.
If a retinaculum tear is suspected, your doctor may recommend the following imaging tests:
- X-rays: These can reveal whether the torn retinaculum has caused an avulsion fracture, where a small piece of the fibula is pulled off. X-rays are also helpful in identifying other potential ankle injuries.
- MRI Scans: MRI imaging can detect abnormal swelling, scar tissue, or tendon tears. However, it may not always confirm the presence of peroneal tendon subluxation.
Treatment: What Are the Options for Peroneal Tendon Subluxation?
Nonsurgical Treatment
Nonsurgical approaches can help manage the symptoms of peroneal tendon subluxation. These treatments aim to control pain, reduce swelling, and improve function. However, in active patients with acute subluxations, nonsurgical methods are only about 50% effective.
Surgical Treatment
For chronic cases of peroneal tendon subluxation that do not respond to nonsurgical measures, surgery is typically required. Surgical intervention aims to correct the underlying issue, such as repairing the damaged retinaculum or stabilizing the tendons to prevent further subluxation.
Nonsurgical Treatment for Peroneal Tendon Subluxation
For acute injuries, nonsurgical treatment may involve immobilizing the ankle in a short-leg cast for 4 to 6 weeks. This approach aims to:
- Allow the torn retinaculum to heal properly.
- Prevent the development of chronic subluxation.
After the cast is removed, your doctor may recommend physical therapy to restore strength, flexibility, and stability in the ankle.
Medications
To manage pain and reduce swelling, your doctor might prescribe anti-inflammatory medications, such as over-the-counter ibuprofen. These medications can help ease symptoms and facilitate a quicker return to normal activities.
Surgical Treatment for Peroneal Tendon Subluxation
When nonsurgical treatments fail to control symptoms, many patients with peroneal tendon subluxation require surgery. Surgical options aim to restore normal anatomy, stabilize the tendons, and prevent further subluxation.
Retinaculum Repair
Retinaculum repair is a popular procedure that restores the normal structure of the retinaculum, which covers and reinforces the peroneal tendon sheath.
- Procedure:
The surgeon makes an incision along the back and lower edge of the fibula bone to access the torn retinaculum.
A burr is used to create a groove (trough) along the fibula near the retinaculum’s original attachment.
The torn retinaculum is pulled into the groove and secured with sutures. The skin is then closed with stitches.
Groove Reconstruction
Groove reconstruction involves deepening the fibular groove to keep the peroneal tendons securely in place.
- Procedure:
An incision is made along the back and lower edge of the fibula.
A small bone flap near the bottom corner of the fibula is cut and folded back like a hinge.
The surgeon removes a small amount of bone beneath the flap to deepen the groove.
The flap is closed, secured in place with a screw, and the tendons are repositioned behind the fibula.
Retinaculum repair may also be performed during this procedure. The skin is then sutured.
Bony Blocks
A bony block creates a physical barrier to prevent the tendons from slipping out of place.
- Procedure:
An incision is made along the lower edge of the fibula.
A small section of the fibula near its lower tip is partially cut and slid backward or rotated to form a barrier.
A screw secures the bony block in its new position.
The surgeon ensures the tendons glide smoothly behind the bony block without slipping. The skin is then closed and sutured.
Each surgical technique is tailored to the patient’s specific condition and anatomy. Post-surgical recovery focuses on restoring function and preventing recurrence of the subluxation.