Pediatric ankle fractures, commonly referred to as broken ankles, are among the most frequent injuries in children. These fractures involve a break in one or more bones of the ankle joint: the tibia (shinbone), the fibula (outer ankle bone), or the talus (a small bone located at the back of the foot).
The severity of ankle fractures in children can vary widely. Minor fractures are often effectively treated with a simple walking boot, while complex fractures may necessitate surgical intervention. A pediatric orthopedic specialist will guide you through the available treatment options and provide ongoing follow-up care to ensure proper healing and monitor long-term recovery outcomes.
Anatomy of the Ankle Joint
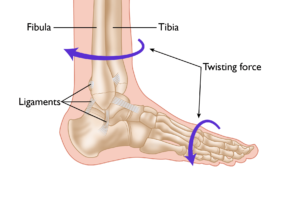
The ankle joint is the point where the tibia (shinbone), fibula (outer ankle bone), and talus (a small bone in the foot) come together. These bones are held in place by ligaments, which function like sturdy ropes, providing stability to the joint by connecting bones and preventing excessive movement. The ankle contains several important ligaments that work together to maintain joint stability and facilitate smooth movement.
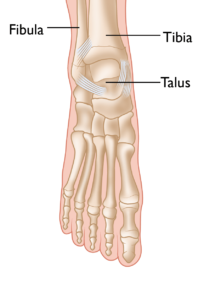 The normal skeletal anatomy of the foot and ankle.
The normal skeletal anatomy of the foot and ankle.
Understanding Ankle Fractures in Children
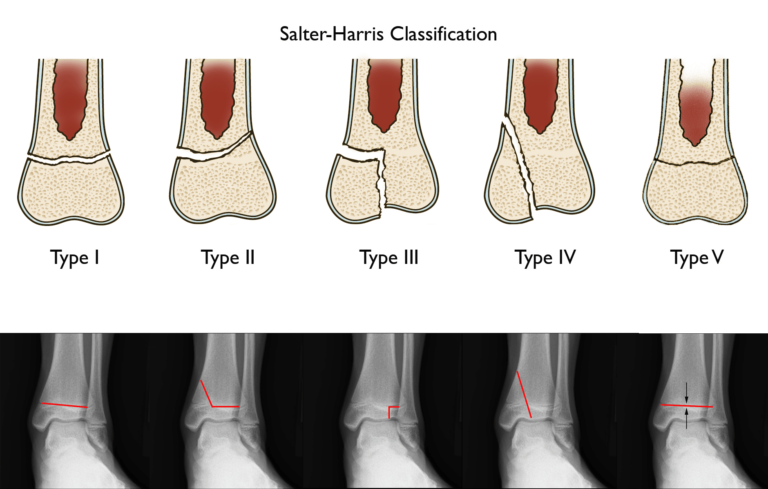
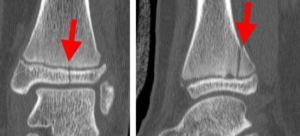
In children and adolescents, ankle fractures typically affect the tibia or fibula, often involving the growth plates—specialized areas of cartilage near the ends of long bones. Growth plates play a critical role in bone development, gradually hardening into solid bone as the child matures. However, because these growth plates are the last parts of the bones to solidify, they are particularly prone to injury and fractures.
As adolescents approach the end of their growth phase, growth plates begin to close and harden, making them susceptible to transitional fractures during this maturing stage. Two common types of transitional ankle fractures are triplane fractures and Tillaux fractures, which require specific treatment approaches depending on their severity and location (refer to the Treatment section for more details)