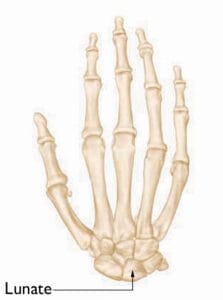
Kienböck’s disease occurs when the blood flow to the lunate, one of the wrist’s small carpal bones, is disrupted. As a living tissue, bone needs a consistent blood supply to stay healthy and functional. When the blood flow is compromised, it can lead to osteonecrosis, where parts or all of the bone tissue die due to a lack of nourishment.
The interruption of blood supply to the lunate weakens its structural integrity, leading to bone collapse. This results in a painful and stiff wrist, and as the condition progresses, it can cause arthritis in the surrounding wrist joints.
Cause
The exact cause of Kienböck’s disease remains unclear, but multiple factors may contribute to the disruption of blood flow to the lunate bone.
Initially, individuals with Kienböck’s disease often mistake it for a wrist sprain, especially if they’ve experienced trauma such as a fall. Such injuries can damage the blood vessels supplying the lunate, leading to compromised circulation.
Certain risk factors can increase the likelihood of developing Kienböck’s disease, including:
- Variations in blood supply: Most people have two arteries supplying the lunate, but some individuals only have one, which can make the bone more susceptible to osteonecrosis.
- Wrist anatomy and bone length differences: The forces exerted on the lunate can vary depending on the relative lengths of the two forearm bones—the radius and ulna. If these bones differ in length, it can place additional pressure on the lunate during certain wrist movements or activities, such as doing push-ups. Over time, this excess pressure can impair blood flow, potentially triggering the onset of Kienböck’s disease.
Symptoms
Kienböck’s disease often presents with the following symptoms:
- Persistent wrist pain
- Swelling around the wrist
- Reduced range of motion or wrist stiffness
- Weakened grip strength
- Tenderness over the lunate, located on the top side of the hand near the middle of the wrist
These symptoms can progressively worsen as the condition advances.
Doctor Examination
Kienböck’s disease is a slowly progressing condition, often taking months or even years to advance. Many individuals don’t seek medical attention until symptoms have persisted for several months or longer.
At the initial consultation, your doctor will review your symptoms and medical history, followed by a physical examination of your hand and wrist.
Diagnosing Kienböck’s disease in its early stages can be challenging because the symptoms closely resemble those of a wrist sprain. Imaging techniques such as X-rays and magnetic resonance imaging (MRI) are essential for diagnosis. However, even with these tools, confirming an early-stage diagnosis can be difficult.
Kienböck’s disease progresses through four distinct stages, each varying in severity. Treatment plans are tailored based on the stage of the disease and other important factors.
Stage I
In the initial stage, symptoms are similar to a wrist sprain, with disrupted blood flow to the lunate. X-rays may appear normal or suggest a possible fracture, while MRI scans are more effective at detecting reduced blood supply, aiding in early diagnosis.
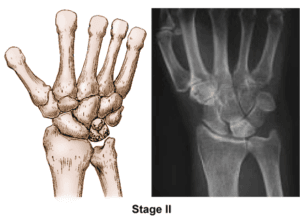
Stage II
During Stage II, the lunate begins to harden due to insufficient blood flow, a process known as sclerosis, which leads to increased bone density. X-rays will show brighter or whiter areas on the lunate, indicating abnormal density. To evaluate the lunate’s condition more accurately, an MRI or computed tomography (CT) scan may be ordered. Common symptoms at this stage include wrist swelling and intermittent pain, especially during activities that put pressure on the wrist, such as weight-bearing exercises.
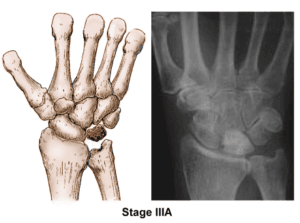
In Stage III, the affected lunate bone starts to collapse and fragment (Stage IIIA). As the bone deteriorates, surrounding carpal bones may shift out of position (Stage IIIB). Patients typically experience worsening pain, weakened grip strength, and decreased wrist mobility during this phase
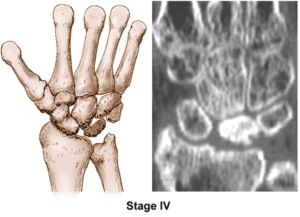
Stage IV
By Stage IV, the collapse of the lunate and the displacement of adjacent bones lead to wrist arthritis. Symptoms mirror those of Stage III, with ongoing wrist pain, limited motion, and reduced grip strength.
Each stage requires different management strategies to slow progression and alleviate symptoms. Let me know if there’s anything else you’d like to modify!
Treatment
While there is no definitive cure for Kienböck’s disease, various treatment options—both nonsurgical and surgical—can help manage the condition based on its stage and the patient’s symptoms. The main objectives are to relieve pressure on the lunate and restore blood flow to the affected bone.
Nonsurgical Treatment
In the earliest stages of the disease, conservative approaches can help alleviate symptoms:
- Pain management: Anti-inflammatory medications such as aspirin or ibuprofen may reduce pain and swelling.
- Wrist immobilization: Temporarily immobilizing the wrist with a splint or cast can help relieve pressure on the lunate.
- Monitoring: Regular observation of symptom changes is important during early-stage treatment. If pain persists or recurs despite these measures, surgical intervention may be considered.
If the diagnosis remains uncertain, your doctor might suggest repeating imaging tests to reassess the condition following initial treatment.
Surgical Treatment
Several surgical options are available, with the choice of procedure depending on the extent of disease progression. Key considerations include the degree of lunate collapse or fragmentation and the presence of joint arthritis. Other factors that influence the decision-making process are the patient’s activity level, treatment goals, symptom tolerance, and the surgeon’s expertise.
Revascularization
In the early stages (Stages I and II), revascularization may be effective in restoring blood flow to the lunate. This procedure involves transferring a bone segment with an attached blood supply, known as a vascularized graft, from another bone—often from the forearm or a neighboring hand bone. The graft is carefully inserted into the lunate while maintaining the integrity of the feeder blood vessel.
To stabilize the bones and reduce pressure during healing, an external fixator or a plate may be used.
- External fixator: A metal device attached to the outside of the wrist with pins inserted into the bones.
- Plate: A metal plate placed under the skin across the wrist joint, attached to the forearm bone and a metacarpal bone in the hand.
Both devices help support the lunate as the graft restores blood flow.
Joint Leveling
If the radius and ulna (forearm bones) are of unequal length, a joint leveling procedure can be performed. This can involve lengthening a bone using a graft or shortening it by removing a section. The goal is to reduce compressive forces on the lunate, potentially halting disease progression.
Proximal Row Carpectomy
For severe cases where the lunate has collapsed or fragmented, a proximal row carpectomy may be necessary. This procedure removes the lunate along with the adjacent carpal bones. It aims to relieve pain while preserving some wrist motion.
Fusion (Arthrodesis)
To alleviate pressure on the lunate, a surgical procedure called fusion, or arthrodesis, may be performed to join nearby wrist bones into a single, solid structure. There are two types of fusion:
- Partial fusion: Involves fusing only some of the wrist bones together, which helps relieve pain while retaining a degree of wrist motion.
- Complete fusion: If the disease has advanced to severe arthritis, all wrist bones may be fused to the radius. This approach effectively relieves pain and enhances hand function, although it eliminates all wrist motion. However, the ability to rotate the forearm remains intact.
Outcomes
The severity and progression rate of Kienböck’s disease can vary widely among individuals. The success of treatment largely depends on the extent of damage to the lunate and the surrounding wrist bones. In some cases, multiple procedures may be needed over time if the condition continues to worsen.
Summary
Kienböck’s disease presents challenges in both diagnosis and treatment. The condition typically progresses slowly and is often not detected until significant wrist pain or functional issues arise.
Treatment strategies are tailored to the stage and severity of the disease, taking into account the condition of the lunate (such as collapse or fragmentation) and the state of surrounding joint surfaces (presence of arthritis).
Although full recovery of normal wrist function is not expected, appropriate treatment can significantly improve long-term pain management and help preserve wrist function.