Knee osteonecrosis, also referred to as avascular necrosis, is a debilitating condition resulting from a disrupted blood supply to a portion of the bone in the femur (thighbone) or tibia (shinbone). Since healthy bone tissue relies on a consistent blood flow for nourishment and repair, the interruption can lead to the deterioration of the knee joint and the development of severe arthritis.
Early diagnosis of knee osteonecrosis allows for less invasive treatment options, such as pain management through medications and reducing stress on the affected knee. However, in more advanced cases, surgical intervention is often necessary to halt further bone damage and restore joint function effectively.
Anatomy
The knee is the largest and most robust joint in the human body. It consists of three key bones: the lower end of the femur (thighbone), the upper end of the tibia (shinbone), and the patella (kneecap). The areas where these bones meet are coated with articular cartilage, a smooth and resilient tissue that cushions the bones and allows seamless movement of the leg by reducing friction.
Knee osteonecrosis is most commonly observed on the inside portion of the knee, known as the medial femoral condyle. However, it can also occur on the outer portion (lateral femoral condyle) or on the flat surface at the top of the shinbone, referred to as the tibial plateau.
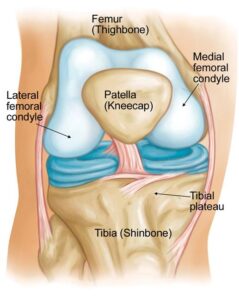 Osteonecrosis of the knee occurs most often in the medial femoral condyle, a segment of bone located at the lower end of the femur (thighbone).
Osteonecrosis of the knee occurs most often in the medial femoral condyle, a segment of bone located at the lower end of the femur (thighbone).
Cause
Osteonecrosis arises when the blood supply to a specific section of bone is interrupted. Without sufficient blood flow, the affected bone tissue dies and begins to collapse. Consequently, the articular cartilage that overlays the bone deteriorates as well, often leading to severe arthritis and impaired joint function.
While osteonecrosis of the knee can develop in individuals of any age, it is more prevalent in people over 60. Women are notably at higher risk, being three times more likely to experience this condition compared to men.
Risk Factors
The exact cause of reduced blood supply to the knee is not always clear, but several factors have been identified that increase the likelihood of developing osteonecrosis:
- Injury: Trauma to the knee, such as a stress fracture or dislocation, can damage blood vessels and impair blood flow to the bone, increasing the risk of osteonecrosis.
- Oral Corticosteroid Medications: Long-term use of oral steroids, commonly prescribed for conditions like asthma and rheumatoid arthritis, is linked to osteonecrosis. Although the exact mechanism is unclear, research indicates that steroid-induced osteonecrosis often affects multiple joints throughout the body.
- Medical Conditions: Certain health conditions, including obesity, sickle cell anemia, and lupus, are associated with a higher risk of knee osteonecrosis. Additionally, individuals undergoing treatment for HIV may experience osteonecrosis due to the effects of antiretroviral medications.
- Transplants: Organ transplant recipients, particularly those who have undergone kidney transplantation, are more prone to developing osteonecrosis.
- Excessive Alcohol Consumption: Chronic alcohol abuse can lead to fatty deposits in blood vessels and increased cortisone levels, both of which reduce blood flow to the bone and contribute to osteonecrosis.
If osteonecrosis is not detected and treated promptly, it can progress to severe osteoarthritis, significantly impairing joint function.
Symptoms
Osteonecrosis progresses through several stages, each with distinct symptoms:
- Early Stage: The initial sign is often a sudden onset of pain on the inside of the knee, which may be triggered by a specific activity or a minor injury.
- Progressive Stage: As the condition worsens, standing, bearing weight, and moving the affected knee become increasingly painful.
Additional symptoms may include:
- Swelling over the front and inner side of the knee
- Tenderness around the knee joint
- Reduced range of motion in the knee
The disease progression can take months to over a year. Early diagnosis is crucial, as studies indicate that prompt treatment leads to more favorable outcomes and may slow or prevent further joint damage.
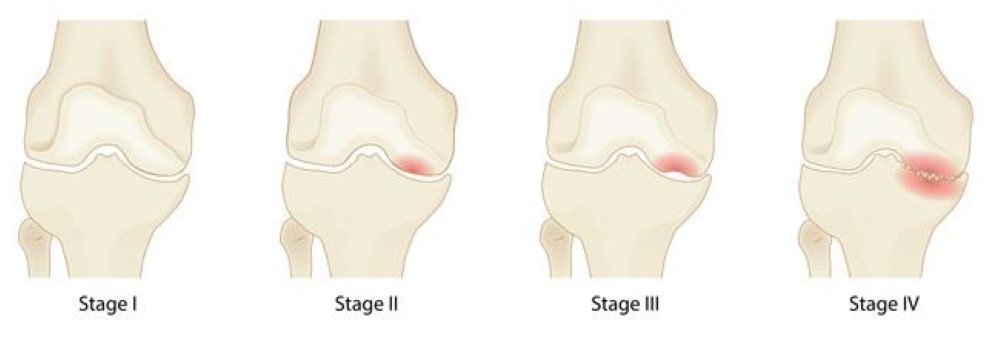 The four stages of osteonecrosis of the knee. The disease can progress from a normal, healthy knee (Stage 1) to the collapse of the bone and severe osteoarthritis (Stage 4).
The four stages of osteonecrosis of the knee. The disease can progress from a normal, healthy knee (Stage 1) to the collapse of the bone and severe osteoarthritis (Stage 4).
Doctor Examination
During a medical evaluation for knee osteonecrosis, your doctor will review your overall health and medical history, followed by a detailed discussion of your symptoms. The physical examination will focus on identifying key signs of the condition, including:
- Joint Swelling, Warmth, or Redness: Indicators of inflammation or underlying joint issues.
- Tenderness: Sensitivity in specific areas around the knee.
- Range of Motion: Assessment of both passive (assisted) and active (self-directed) movement to evaluate joint flexibility and stiffness.
- Joint Instability: Examination to detect any instability or weakness in the knee joint.
- Pain Under Weight-Bearing Conditions: Observation of discomfort when pressure or weight is applied to the knee.
- Muscle, Tendon, and Ligament Health: Checking for any injuries or abnormalities in the surrounding soft tissues.
 During the exam, your doctor will look for areas of tenderness about your knee.
During the exam, your doctor will look for areas of tenderness about your knee.
Imaging Studies
Imaging techniques play a crucial role in confirming a diagnosis of osteonecrosis.
- X-rays: X-rays create detailed images of dense structures like bones. These are often used to identify changes in bone structure that occur during the later stages of osteonecrosis. However, in the early stages of the condition, X-ray results typically appear normal, which may necessitate additional imaging for accurate diagnosis.
Advanced imaging methods, such as MRI or CT scans, may also be considered to detect early signs of osteonecrosis and assess the extent of bone damage. Early detection through imaging can significantly impact treatment outcomes.
 X-ray shows osteonecrosis at the lower end of the femur (thighbone) in the medial femoral condyle.
X-ray shows osteonecrosis at the lower end of the femur (thighbone) in the medial femoral condyle.
Magnetic Resonance Imaging (MRI) Scans
MRI scans are highly effective in detecting early changes in bone tissue that might not be visible on X-rays. This advanced imaging technique is particularly useful in evaluating the extent of bone damage caused by osteonecrosis.
- Early Detection: MRI scans can reveal subtle signs of osteonecrosis, even before symptoms appear. This makes it a critical tool for identifying the disease in its early stages, which can lead to more effective intervention.
- Assessment of Disease Spread: An MRI can determine how much of the bone is affected and may also identify osteonecrosis developing in other areas, such as the opposite knee joint, even if it has not yet caused symptoms.
The detailed insights provided by MRI scans are invaluable for diagnosing osteonecrosis accurately and planning the most appropriate treatment strategy.
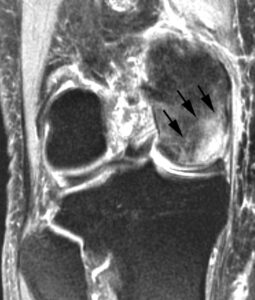 This MRI scan shows osteonecrosis in the medial femoral condyle. An MRI is often used to detect early symptoms of the disease.
This MRI scan shows osteonecrosis in the medial femoral condyle. An MRI is often used to detect early symptoms of the disease.
Bone Scan
In certain cases, your doctor may recommend a bone scan to aid in the diagnosis of osteonecrosis. This diagnostic test involves injecting a small amount of radioactive dye into a vein.
- How It Works: The radioactive material travels through the bloodstream and is absorbed by active bone tissue. Areas affected by osteonecrosis often show an increased uptake of the radioactive dye due to heightened bone activity associated with the condition.
- Purpose: A bone scan provides detailed information about the metabolic activity in the bone, helping to identify areas of damage or abnormality that may not be evident on other imaging studies.
Treatment for Osteonecrosis of the Knee
The treatment approach for osteonecrosis depends on several factors, including:
- The stage of the disease
- The extent of bone damage
- The underlying cause of the condition
Nonsurgical Treatment
In the early stages of osteonecrosis, nonsurgical interventions are often sufficient, particularly if the affected area is small. These treatments aim to relieve symptoms and slow disease progression.
1. Medications
- Nonsteroidal Anti-Inflammatory Drugs (NSAIDs): Medications such as ibuprofen and naproxen can help reduce pain and inflammation in the knee.
- Bisphosphonates: These drugs may be considered, especially for younger patients, to help preserve bone density and prevent further damage.
2. Reduced Weight Bearing
- Avoiding pressure on the affected knee can facilitate healing and minimize further damage.
- Crutches: Your doctor may recommend using crutches temporarily to offload weight from the joint.
- “Unloader” Brace: In some cases, wearing a specialized brace can help shift weight away from the damaged area of the knee, reducing joint stress.
3. Exercise
- A customized exercise program designed by your doctor or physical therapist can help strengthen the thigh muscles and maintain joint mobility.
- Water Exercises: For patients needing low-impact activity, water-based exercises can help improve muscle strength without placing undue stress on the knee joint.
4. Activity Modification
- Avoiding activities that exacerbate pain or stress the knee joint can help prevent worsening of symptoms.
Surgical Treatment
If a significant portion of the bone is damaged or nonsurgical treatments fail to provide relief, surgery may be necessary. Various procedures are available depending on the severity and location of the osteonecrosis.
1. Arthroscopic Debridement and Microfracture
- Debridement: This minimally invasive procedure involves using a small camera and surgical tools to remove loose bone fragments or damaged cartilage from the joint.
- Microfracture: For smaller lesions, the surgeon may create tiny holes in the underlying bone to enhance blood flow and stimulate healing.
2. Core Decompression
- This procedure involves drilling one or more holes into the affected bone to alleviate pressure, improve circulation, and encourage the growth of new blood vessels.
- Early Diagnosis Benefit: When performed in the early stages of osteonecrosis, core decompression can prevent bone collapse and the progression to arthritis.
Both nonsurgical and surgical treatments aim to preserve joint function, alleviate pain, and improve overall quality of life. Early detection and treatment are crucial for achieving the best possible outcomes.
Advanced Surgical Treatments for Osteonecrosis
1. Osteochondral (Bone and Cartilage) Grafting
Core decompression is often paired with bone and cartilage grafting to stimulate the regeneration of healthy bone and provide structural support to the cartilage in the knee joint.
- Bone Grafts: Healthy bone tissue can be transplanted from a donor (allograft) or harvested from another part of the patient’s body (autograft).
- Synthetic Options: Several synthetic bone graft materials are also available and can be used as alternatives to natural grafts.
2. Autologous Chondrocyte Implantation (ACI)
This is a two-step procedure designed to restore damaged cartilage in the knee:
- Step 1: During an arthroscopic procedure, a small sample of cartilage-producing cells (chondrocytes) is harvested from the knee. These cells are then cultured in a laboratory for several weeks to multiply.
- Step 2: The cultured chondrocytes are re-implanted into the knee at the site of cartilage loss. These cells grow within the joint, regenerating healthy cartilage and restoring function.
3. Osteotomy
Osteotomy involves reshaping the tibia (shinbone) or femur (thighbone) to redistribute weight away from the damaged portion of the knee joint.
- The surgeon may remove a portion of the bone or insert a wedge of bone graft or synthetic material to achieve the desired alignment.
- This procedure reduces pain and improves function by shifting weight off the damaged area.
4. Total or Partial Knee Replacement
For advanced cases where the bone has collapsed, knee replacement surgery may be necessary.
- Total Knee Replacement: The damaged bone and cartilage are removed, and the joint is reconstructed using metal or plastic prosthetic components.
- Unicompartmental (Partial) Knee Replacement: If the damage is limited to a specific area of the knee, only the affected compartment is replaced, preserving more of the natural joint structure.
Expected Outcomes
Most patients experience significant pain relief and improved knee function following treatment for osteonecrosis. However, outcomes can vary depending on the stage of the disease at diagnosis and the chosen treatment approach. Your doctor will provide personalized guidance and discuss the expected results based on your specific condition.