Plantar fasciitis, a prevalent condition affecting the heel, is among the leading causes of foot pain, particularly on the sole. Each year, nearly 2 million individuals seek treatment for this condition, highlighting its widespread impact.
This condition arises when the plantar fascia—a robust, fibrous tissue that runs along the bottom of the foot, supporting the arch—becomes inflamed and irritated.
Anatomy
The plantar fascia is a slender, elongated ligament positioned just beneath the skin on the underside of the foot. This crucial structure links the heel bone to the forefoot and plays a vital role in supporting the foot’s arch, ensuring stability and proper movement.
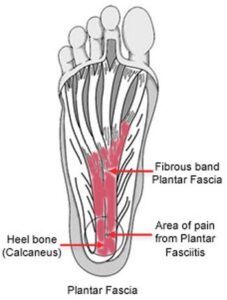 The plantar fascia is a ligament that lies beneath the skin on the bottom of your foot.
The plantar fascia is a ligament that lies beneath the skin on the bottom of your foot.
Cause
The plantar fascia is built to withstand significant stress and strain, especially during activities like walking, running, or sports. However, excessive or repetitive pressure can lead to tissue damage or small tears. This triggers the body’s natural inflammatory response, resulting in heel pain and stiffness commonly associated with plantar fasciitis.
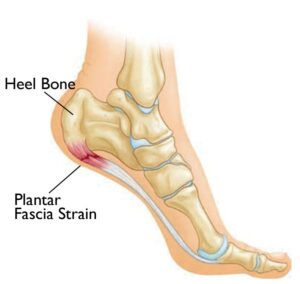 Too much pressure on the plantar fascia can damage or tear the tissues, causing heel pain.
Too much pressure on the plantar fascia can damage or tear the tissues, causing heel pain.
Risk Factors
Plantar fasciitis often develops without a clear or specific cause. However, several factors can increase the likelihood of experiencing this condition:
- Changes or Increases in Activity: Starting a new exercise routine or significantly increasing physical activity can strain the plantar fascia.
- Repetitive High-Impact Movements: Activities like running, dancing, or playing high-impact sports place consistent stress on the foot.
- Prolonged Standing on Hard Surfaces: Jobs that require standing for extended periods, such as nursing, factory work, or teaching, heighten the risk.
- Foot Anatomy: Structural issues like flat feet or high arches can contribute to abnormal stress on the plantar fascia.
- Tight Calf Muscles: Limited flexibility in the calf muscles can increase strain on the foot’s arch.
- Obesity: Excess body weight adds pressure on the foot, increasing the risk of inflammation.
- Age: Individuals between the ages of 40 and 60 are more commonly affected by plantar fasciitis.
Symptoms
The hallmark symptoms of plantar fasciitis include:
- Heel Pain: Discomfort localized at the bottom of the foot near the heel.
- Morning Stiffness: Pain that is most noticeable with the first few steps after waking up or after extended periods of inactivity, such as sitting or driving. This pain typically subsides after a few minutes of walking.
- Post-Activity Pain: Increased pain after physical activity or exercise, rather than during the activity itself.
Doctor Examination
During a consultation, your doctor will evaluate your symptoms and perform a thorough physical examination of your foot. Key factors they will assess include:
- Foot Structure: Presence of a high arch or flat foot.
- Pain Points: Identification of the most tender area on the sole, typically located just in front of the heel bone.
- Range of Motion: Checking for limited dorsiflexion, or restricted upward movement, of the ankle.
- Exclusion of Other Conditions: Ensuring symptoms are not caused by related issues such as insertional Achilles tendinitis, heel stress fractures, or plantar nerve entrapment.
Diagnostic Tests
Imaging tests may be recommended to confirm the diagnosis of plantar fasciitis and rule out other potential causes of heel pain.
- X-Rays: These provide detailed images of the bones, helping to exclude conditions such as fractures or arthritis.
- Heel Spurs: X-rays can reveal heel spurs, which may develop from prolonged tension at the plantar fascia’s attachment point on the heel bone. However, heel spurs are not the direct cause of plantar fasciitis pain and typically do not require removal for treatment.
 Heel spurs do not cause plantar fasciitis pain.
Heel spurs do not cause plantar fasciitis pain.
Other Imaging Tests
While magnetic resonance imaging (MRI) and ultrasound are available for diagnosing plantar fasciitis, they are not commonly utilized. These advanced imaging techniques are typically reserved for specific cases:
- MRI: May be recommended if initial treatments fail to alleviate heel pain or if your doctor suspects another underlying condition contributing to the symptoms.
Treatment
Nonsurgical Treatment
Over 90% of individuals with plantar fasciitis experience significant improvement within 10 months when following simple, non-invasive treatment approaches.
- Rest: Minimizing or ceasing activities that exacerbate heel pain is crucial. High-impact activities such as running, dancing, or aerobics should be avoided. In some cases, your doctor may suggest using a walking boot or crutches temporarily to allow the foot to heal.
- Activity Modification: Switching to low-impact exercises like cycling or swimming can reduce stress on the feet and joints while maintaining physical activity.
- Stretching: Tight calf muscles and plantar fascia often worsen the symptoms of plantar fasciitis. Regular stretching exercises targeting the calves and plantar fascia are highly effective in reducing pain and promoting recovery.
Calf Stretch Exercise
Performing calf stretches can help alleviate the tension in your calf muscles and heel cord, which often contributes to plantar fasciitis. Follow these steps:
- Stand facing a wall, placing your hands on the wall for support.
- Extend one leg behind you, keeping the knee straight and the heel firmly on the ground.
- Position the other leg in front, bending the knee slightly.
- Slowly push your hips toward the wall, maintaining control to stretch the calf muscle and heel cord of the extended leg.
- Hold the stretch for 10 seconds, then relax.
- Repeat this exercise 20 times for each foot.
Plantar Fascia Stretch
Performing a plantar fascia stretch helps improve flexibility and relieve tension in the foot. Follow these steps:
- Sit comfortably in a chair and cross the affected foot over the opposite knee.
- Using your hand, grasp the toes of the affected foot and gently pull them toward you in a controlled manner.
- If you have trouble reaching your toes, use a towel looped around your big toe to assist.
- With your other hand, feel along the bottom of your foot for the plantar fascia, which will feel like a tight band during the stretch.
- Hold the stretch for 10 seconds and then release.
- Repeat this exercise 20 times for each foot.
This stretch is most effective when performed in the morning before standing or walking.
Ice Therapy
Rolling your foot over a chilled water bottle or an ice pack for 20 minutes provides relief from pain and reduces inflammation. This can be done 3 to 4 times daily for maximum benefit.
Nonsteroidal Anti-Inflammatory Drugs (NSAIDs)
Over-the-counter medications like ibuprofen or naproxen can help manage pain and inflammation. However, prolonged use beyond one month should be discussed with your primary care physician.
Physical Therapy
Your doctor may recommend working with a physical therapist who will design an exercise program tailored to stretch the calf muscles and plantar fascia. Physical therapy may also include specialized treatments such as:
- Ice application
- Massage
- Techniques to reduce inflammation
These interventions work together to decrease plantar fasciitis symptoms effectively.
Supportive Shoes and Orthotics
Proper footwear is essential for managing plantar fasciitis. Consider the following:
- Shoes with Cushioning: Thick-soled shoes with extra padding can alleviate tension on the plantar fascia caused by the repetitive microtrauma of walking.
- Heel Pads: Affordable silicone heel pads elevate and cushion the heel, reducing strain.
- Orthotics: Pre-made or custom shoe inserts provide additional arch support.
- Avoid Unsupportive Footwear: Worn-out or unsupportive shoes exacerbate symptoms, so replace old athletic shoes before they lose their cushioning and support.
Night Splints
Night splints, worn while sleeping, help keep the foot in a dorsiflexed position (toes pointing upward). This stretches the plantar fascia and prevents it from relaxing overnight, reducing morning heel pain. Although it may take time to adjust to wearing a night splint, it is highly effective for relieving plantar fasciitis symptoms.
 Soft heel pads can provide extra support.
Soft heel pads can provide extra support.
Other Treatments
If symptoms persist after several months of nonsurgical interventions, your doctor may recommend the following advanced procedures:
Casting
A custom-molded cast can immobilize the foot, creating an optimal healing environment by preventing movement. Unlike a removable boot, a cast ensures consistent immobilization and may be more effective for some patients.
Cortisone Injections
Cortisone, a potent anti-inflammatory steroid, can be injected into the plantar fascia to reduce inflammation and alleviate pain. However, this treatment carries risks, as repeated injections may weaken the plantar fascia and increase the likelihood of rupture, leading to chronic pain and foot flattening.
Platelet-Rich Plasma (PRP) Injections
PRP therapy involves extracting platelets from the patient’s blood and injecting them into the plantar fascia to stimulate healing. While PRP carries no risk of fascia rupture, it is often expensive, and further research is needed to confirm its long-term effectiveness.
Extracorporeal Shockwave Therapy (ESWT)
This noninvasive procedure uses high-energy shockwave impulses to stimulate tissue repair in the plantar fascia. While ESWT has minimal risks, its effectiveness varies, and it is typically considered before surgical options.
Ultrasonic Tissue Repair
This minimally invasive technique uses ultrasound imaging to guide a vibrating probe to the affected area. The probe breaks down and removes damaged tissue, providing relief for patients with chronic plantar fasciitis.
Surgical Treatment
Surgery is typically reserved for patients who have not improved after 12 months of aggressive nonsurgical treatments.
Gastrocnemius Recession
This procedure involves surgically lengthening one of the two muscles in the calf (gastrocnemius) to reduce tension on the plantar fascia. It is particularly beneficial for patients with tight calf muscles who struggle to flex their feet despite extensive stretching efforts.
- Procedure: The surgery can be performed through a traditional open incision or a smaller incision using an endoscope (a small camera-guided instrument).
- Complications: Potential risks include damage to the sural nerve and calf weakness, though complication rates are generally low.
Partial Plantar Fascia Release
Often performed in conjunction with a gastrocnemius recession, this procedure involves partially cutting the plantar fascia at its attachment point on the heel bone to relieve tension. Large bone spurs, if present, may also be removed during this surgery.
- Procedure Options: The surgery can be performed through an open incision or endoscopically. However, endoscopic surgery carries a higher risk of nerve damage than open surgery.
- Complications: Common risks include nerve damage and incomplete pain relief.
Recovery
After surgery, patients typically require a short period of protected weight-bearing to allow the incision to heal properly. Most individuals experience good outcomes, though there is a risk of chronic pain or dissatisfaction. Surgery is recommended only after exhausting all nonsurgical treatment options.