A calcaneus fracture, commonly known as a heel bone fracture, is a serious and often debilitating injury. These fractures typically result from high-impact incidents, such as motor vehicle accidents or falls from significant heights, where the heel absorbs the body’s full weight, causing it to crush. This trauma can lead to significant structural changes, including the widening, shortening, or deformity of the heel.
Calcaneus fractures are often complex injuries requiring prompt and effective treatment. Surgical intervention is frequently necessary to reconstruct the heel’s anatomy and restore functionality, enabling patients to regain mobility and resume daily activities. However, even with advanced treatment methods, long-term complications may arise. These can include persistent pain, swelling, reduced range of motion, and the development of arthritis. Additionally, individuals in physically demanding professions may face challenges in returning to work due to the lasting effects of this injury.
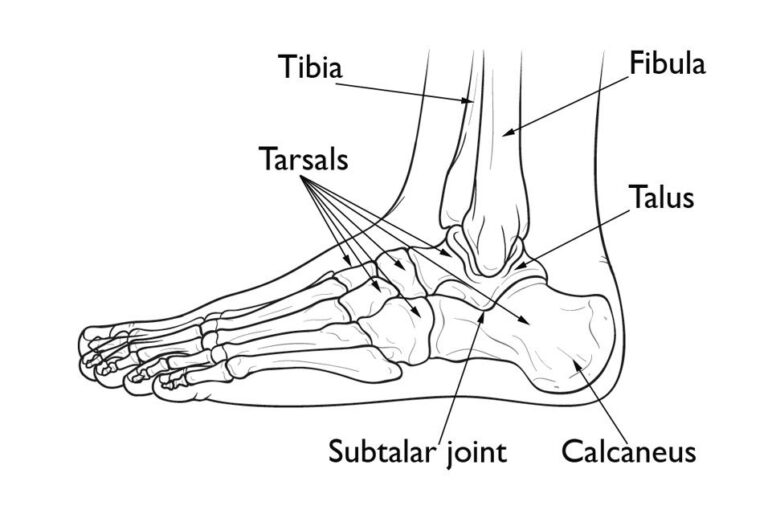
Anatomy of the Foot
The bones of the foot are categorized into three distinct sections:
- Hindfoot
- Midfoot
- Forefoot
The hindfoot and midfoot are comprised of seven bones known as tarsals. The calcaneus, or heel bone, is the largest of these tarsal bones. Positioned at the back of the foot (hindfoot), the calcaneus lies beneath the three bones that form the ankle joint:
- Tibia (shinbone)
- Fibula (the smaller bone of the lower leg)
- Talus (a small bone that acts as a hinge between the tibia and fibula)
Together, the calcaneus and talus form the subtalar joint, which plays a crucial role in facilitating side-to-side movement of the hindfoot, essential for maintaining balance on uneven surfaces.
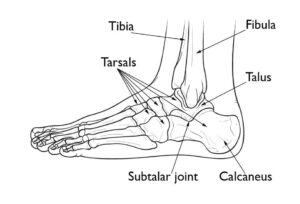 Normal foot anatomy. Together, the calcaneus (heel bone) and talus form the subtalar joint, which moves the foot side to side in walking.
Normal foot anatomy. Together, the calcaneus (heel bone) and talus form the subtalar joint, which moves the foot side to side in walking.
Overview of Calcaneus Fractures
Calcaneus fractures are relatively rare, accounting for only about 2% of all fractures in adults. Even among fractures of the tarsal bones, calcaneus fractures make up only half of these cases.
When the heel bone fractures, it often becomes wider and shorter. In many instances, the fracture extends into the subtalar joint. This can damage the articular cartilage that lines the joint, leading to long-term complications such as chronic pain, arthritis, and restricted mobility.
Severity of Calcaneus Fractures
The severity of a calcaneus fracture depends on various factors, including:
- The number of fractures in the bone.
- Size and displacement of the bone fragments. In some cases, the fragments remain aligned, while in severe fractures, they may shift significantly or overlap.
- Damage to the cartilage in the subtalar joint.
- Injury to surrounding soft tissues, such as muscles, tendons, and skin.
In cases where the bone fragments penetrate through the skin or when a wound reaches the bone, the injury is classified as an open fracture. These fractures are more severe because they cause greater damage to surrounding tissues and carry a higher risk of infection in both the wound and the bone itself. Prompt medical attention to clean the wound is critical to prevent complications and ensure proper healing.
Causes of Calcaneus Fractures
Calcaneus fractures typically occur as a result of high-impact trauma, such as a fall from a significant height or a motor vehicle collision. The severity of these fractures can range widely, depending on the force involved. For instance:
- A minor twist of the ankle may cause a small crack in the bone.
- A high-impact event, like a head-on car collision, can result in a comminuted fracture, where the bone is shattered into multiple pieces.
Common Mechanisms of Injury
The calcaneus can sustain similar fracture patterns from different types of trauma. Two primary mechanisms include:
- Falls from Heights:
When an individual lands on their feet after a fall, the body’s weight drives the talus bone downward into the calcaneus, causing the heel bone to fracture. - Motor Vehicle Collisions:
In car accidents, the force of the impact often drives the calcaneus upward against the talus when the heel is crushed against the floorboard.
In both scenarios, the greater the force of impact, the more extensive the damage to the calcaneus.
Associated Injuries in High-Energy Fractures
High-energy calcaneus fractures often occur in conjunction with other serious injuries. Commonly associated injuries include fractures of the spine, hip, or even the opposite heel. These additional injuries highlight the need for a comprehensive evaluation and treatment plan following significant trauma.
 (Left) In some injuries, the talus is forced downward and acts like a wedge to fracture the calcaneus. (Right) This computerized reconstruction of a calcaneus fracture shows the amount of damage that can occur.
(Left) In some injuries, the talus is forced downward and acts like a wedge to fracture the calcaneus. (Right) This computerized reconstruction of a calcaneus fracture shows the amount of damage that can occur.
Symptoms of Calcaneus Fractures
Patients with calcaneus fractures commonly experience the following symptoms:
- Severe pain in the heel.
- Bruising and discoloration around the injury.
- Swelling of the foot and ankle.
- Deformity of the heel.
- Difficulty bearing weight on the heel or walking.
In cases of minor fractures, pain may not completely restrict walking, but patients often limp. This occurs because the Achilles tendon, which relies on the calcaneus to support body weight, loses its ability to function effectively if the heel bone is deformed. Consequently, the foot and ankle feel unstable, leading to an altered walking pattern.
Doctor’s Examination of Calcaneus Fractures
Providing Background Information
During your consultation, it is essential to describe the circumstances of your injury in detail. For example, if you fell from a height, specify the distance and the type of surface you landed on. Additionally, inform your doctor about other health conditions (e.g., diabetes) and any medications or lifestyle factors, such as smoking, which may influence your recovery.
Physical Examination
Your doctor will evaluate your symptoms and medical history, followed by a thorough physical examination. They will:
- Inspect your foot and ankle for skin damage or puncture wounds.
- Assess blood flow to the foot by checking the pulse at key points.
- Test for nerve function by determining if you can move your toes and feel sensations on the bottom of your foot.
- Examine other parts of the injured leg, the opposite leg, pelvis, and spine for additional injuries.
Diagnostic Tests for Calcaneus Fractures
X-rays
X-rays are the most common diagnostic tool used to confirm a calcaneus fracture. They provide clear images of dense structures, such as bones, revealing the fracture’s location and whether the bones are displaced.
CT Scans
A CT scan offers more detailed imaging, particularly valuable given the calcaneus’s complex anatomy. CT scans help evaluate the fracture’s severity, providing critical information to guide the treatment plan. Your doctor may review these images with you to help you understand your injury.
Treatment Options for Calcaneus Fractures
Your doctor will develop a treatment plan based on several factors, including the cause of the injury, your overall health, the severity of the fracture, and the extent of soft tissue damage. The primary goal is to restore the calcaneus’s normal anatomy, as this is associated with better long-term outcomes.
Nonsurgical Treatment
Nonsurgical treatment is recommended if the fractured bone fragments remain in proper alignment.
- Immobilization: A cast, splint, or brace will hold the bone in position during healing. Typically, you will wear a cast for 6 to 8 weeks (or longer) and avoid putting weight on the foot until the bone has healed completely.
Surgical Treatment
Surgery may be necessary if the bone fragments are displaced. While surgery can restore the calcaneus’s normal shape, it carries risks, including wound healing issues, infection, and nerve damage.
- Timing of Surgery: If swelling is significant but the skin remains intact, surgery may be delayed until the swelling subsides. This is often achieved by elevating the leg and immobilizing it for several days, which helps reduce complications and improve recovery.
- Emergency Surgery: Open fractures, where bone fragments are exposed, require immediate surgery to clean the wound and remove damaged tissue to prevent infection.
Surgical Procedures
- Percutaneous Screw Fixation: When bone fragments are large and can be realigned without a large incision, screws are inserted through small incisions to stabilize the fracture.
 (Left) A displaced fracture of the calcaneus. (Right) The fracture has been reduced and the bones held in place with screws.
(Left) A displaced fracture of the calcaneus. (Right) The fracture has been reduced and the bones held in place with screws.
Open Reduction and Internal Fixation for Calcaneus Fractures
Open Reduction and Internal Fixation (ORIF) is a common surgical technique used to treat calcaneus fractures where the bones are significantly displaced. This procedure involves:
- Open Incision:
The surgeon makes an incision to access the fractured calcaneus. - Reduction of Bones:
The displaced bone fragments are carefully repositioned into their correct anatomical alignment. - Stabilization with Hardware:
Once aligned, the bones are secured using wires, metal plates, and screws to maintain their position during the healing process.
This method effectively restores the calcaneus’s normal shape and structure, improving the patient’s ability to walk and bear weight. However, as with any surgical procedure, ORIF carries risks such as infection, wound healing complications, and hardware-related issues, which your doctor will discuss with you in detail.
 In this X-ray, the bone fragments have been realigned and held in place with metal plates and screws.
In this X-ray, the bone fragments have been realigned and held in place with metal plates and screws.
Recovery and Rehabilitation for Calcaneus Fractures
Healing Process
Bones possess an incredible ability to heal, but the severity of a calcaneus fracture greatly influences recovery time. More severe fractures often result in prolonged healing and an increased risk of permanent functional loss, regardless of the treatment method.
Pain Management After Treatment
Post-surgical pain is a natural part of the recovery process. Effective pain management can facilitate faster healing and improve overall recovery.
Medications for Pain Relief
Doctors typically prescribe medications to manage short-term pain after surgery, including:
- Opioids: Powerful pain relievers used for short durations.
- Non-steroidal anti-inflammatory drugs (NSAIDs): Help reduce pain and inflammation.
- Local anesthetics: Provide targeted relief.
A combination of these medications may be used to optimize pain management while minimizing opioid dependence.
Important Note on Opioids: Opioids can be addictive, and their misuse has become a significant public health concern. Follow your doctor’s instructions carefully and discontinue use as soon as your pain improves. If pain persists beyond a few days, consult your healthcare provider.
Rehabilitation Process
Whether treated surgically or nonsurgically, rehabilitation is essential for recovery. The duration of rehabilitation depends on the fracture’s severity and whether other injuries are present.
Key Aspects of Rehabilitation
- Early Motion
Early movement of the foot and ankle is often encouraged to prevent stiffness and promote healing. If surgery was performed, movement may be initiated once the wound has sufficiently healed. - Physical Therapy
A structured physical therapy program focuses on exercises to:- Improve the range of motion in the foot and ankle.
- Strengthen supporting muscles.
- Enhance overall mobility.
While these exercises may be painful initially, they are crucial for regaining normal function and returning to daily activities.
- Weight-Bearing Activities
- Most patients must avoid putting weight on the heel for approximately 3 months after injury or surgery. Partial weight-bearing may begin within 6 to 10 weeks in some cases.
- Walking aids, such as crutches, a cane, or a walker, may be necessary during this period.
- A specialized boot is often used to provide support.
Risks of Premature Weight-Bearing
Placing weight on the foot too soon can disrupt the healing process:
- Bone fragments may shift, potentially requiring additional surgery.
- If surgery has been performed, screws may loosen or break, and the bone could collapse.
- While the initial weight-bearing attempt may seem uneventful, continued pressure on an unhealed bone can lead to hardware failure and delayed recovery.
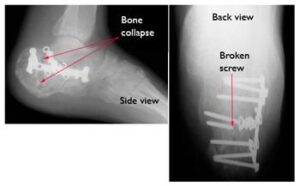 Six months after surgery, this patient’s hardware has failed. Several screws have broken and the calcaneus has collapsed. This patient required major reconstruction, and today walks with a limp and has little motion in the foot.
Six months after surgery, this patient’s hardware has failed. Several screws have broken and the calcaneus has collapsed. This patient required major reconstruction, and today walks with a limp and has little motion in the foot.
Complications of Calcaneus Fractures
Complications are relatively common with calcaneus fractures, ranging from minor issues to more severe outcomes.
Minor Complications
- Delayed Wound Healing: Small or temporary delays in healing around the incision site.
- Nerve Irritation: Irritation of nerves near the surgical site, which may cause discomfort.
- Tendon Irritation: Inflammation or irritation of tendons near the heel.
- Joint Stiffness: Reduced range of motion in the foot and ankle joints.
- Chronic Pain: Persistent discomfort in the heel region.
- Chronic Swelling: Ongoing inflammation and fluid retention around the affected area.
Major Complications
- Wound Healing Failure: Complete failure of the wound to heal properly.
- Infection: Infections in the bone or surrounding tissues, often requiring prompt medical intervention.
- Posttraumatic Arthritis: Joint degeneration following the injury, which can occur with or without surgical treatment.
Impact of Smoking on Healing
Smoking significantly impairs both bone and wound healing. Patients who smoke may experience delayed recovery and a higher risk of complications. If you are a smoker, it is crucial to inform your doctor and discuss strategies to improve healing outcomes.
Related Resources:
Addressing Severe Complications
Infections or complications related to wound healing often require additional surgery to resolve the issue. In rare cases where these complications persist despite treatment, an amputation may be necessary as a last resort.
Outcomes of Calcaneus Fracture Recovery
The recovery timeline for a calcaneus fracture largely depends on the severity of the injury.
- Minor Fractures: Patients with minor fractures, such as small cracks in the bone with minimal muscle damage, may resume normal activities within 3 to 4 months after surgery.
- Severe Fractures: Recovery from severe fractures can take 1 to 2 years and may involve permanent changes in foot and ankle motion.
Despite best efforts, full restoration of pre-injury function and motion is rare in severe cases. While individuals with less physically demanding lifestyles might tolerate these changes, those whose work or hobbies require significant walking or climbing may need to adjust their careers or recreational activities.
Common Post-Recovery Challenges
Some patients experience long-term issues after a calcaneus fracture, including:
- Skin Irritation: Footwear may irritate the skin or tendons around the affected area.
- Altered Gait: If the foot’s arch or Achilles tendon position is not fully restored, walking may be affected, especially on uneven surfaces like grassy fields or hills. Full motion between the talus and calcaneus is rarely regained.
- Pain:
- Subtalar joint pain and limited motion are common, even if the heel’s anatomy is properly restored.
- Persistent discomfort can result from soft tissue damage, residual fracture displacement, arthritis, or hardware irritation from plates or screws.
Further Treatment Options
For patients with ongoing pain or complications, additional treatment may be necessary:
- Orthotics:
- Shoe modifications such as heel pads, lifts, or cups can alleviate chronic issues.
- Special footwear with extra toe compartment depth may also help.
- Additional Surgery:
- If the bone has healed in a deformed position or the subtalar joint develops arthritis, joint fusion surgery may be required. This involves fusing the talus and calcaneus to form one bone, reducing pain but limiting hindfoot motion.
- In cases of severe deformity, corrective surgery may also address alignment issues alongside the fusion.
Improving Outcomes
There is no universal consensus among experts regarding the optimal treatment for calcaneus fractures. Recovery outcomes can vary significantly:
- Patients with normal heel anatomy on X-rays may still experience ongoing symptoms.
- Conversely, some individuals with noticeable deformities on X-rays report minimal symptoms.
Research comparing surgical and nonsurgical treatments has shown mixed results, with the benefits of surgery depending on the patient’s specific circumstances. Studies are ongoing to improve treatment methods, especially for high-risk patients, such as smokers or those with underlying health conditions.
Your doctor will work with you to determine the best treatment plan tailored to your injury and overall health.