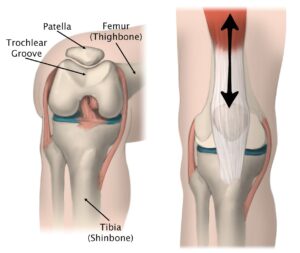
The kneecap, or patella, typically rests securely within a groove at the lower end of the thighbone (femur), moving smoothly up and down as the knee bends and straightens. However, certain incidents, such as a fall or direct impact, can cause the patella to slide too far to the side, leading to a partial or complete dislocation.
A dislocated kneecap often results in immediate pain, reduced knee function, and discomfort. Even if the patella realigns itself naturally, medical evaluation is crucial. Seeking prompt care helps address persistent symptoms and ensures that any potential damage to the knee joint or surrounding soft tissues is properly assessed and treated.
This revised content is optimized for search engines and keeps the scientific information intact while being engaging and informative for readers.
(Left) The patella normally rests in a small groove at the end of the femur called the trochlear groove. (Right) As you bend and straighten your knee, the patella slides up and down within the groove.
Causes of Patellar Dislocation in Children
Several factors can lead to patellar instability or dislocation in children. Often, the kneecap can dislocate with minimal force due to structural irregularities in the knee.
- Structural Abnormalities: A shallow or uneven groove in the femur increases the likelihood of dislocation.
- Ligament Laxity: Children with naturally looser ligaments have highly flexible joints, making them more prone to patellar instability. This condition is more common in girls and often affects both knees.
- Neurological and Developmental Conditions: Children with cerebral palsy or Down syndrome frequently experience patellar dislocations due to muscle imbalances and weakness.
- Congenital Instability: In rare cases, children are born with unstable kneecaps, causing recurrent dislocations from a very young age, often without significant pain.
For children with normal knee structure, patellar dislocations are typically caused by external trauma, such as a direct blow or fall, and are more common in high-impact sports like football. However, dislocations can also occur without direct contact. For example, a right-handed baseball player might dislocate their right kneecap while swinging a bat. As the torso rotates and the foot remains firmly planted, the patella may lag behind, leading to dislocation.
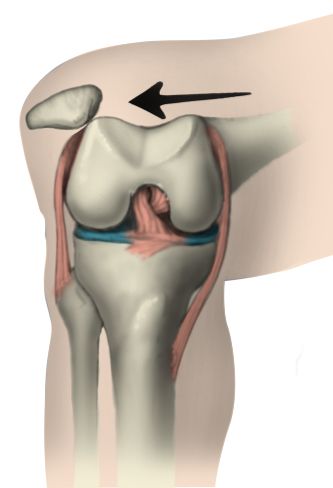
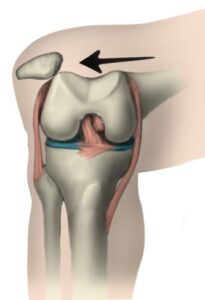
Many things can cause patellar dislocation, such as a shallow groove in the femur or direct force on the knee joint.
Symptoms of Patellar Dislocation
The symptoms of a patellar dislocation vary depending on the extent of the displacement and the degree of damage caused. Common signs to watch for include:
- Pain: Sudden and sharp pain in the knee.
- Kneecap Movement: A sensation of the kneecap shifting or sliding out of its groove.
- Instability: Feeling the knee buckle or give way during movement.
- Popping Sound: Hearing a noticeable “pop” when the kneecap dislocates.
- Swelling: Visible swelling around the knee joint.
- Deformity: A misshapen or abnormal appearance of the knee.
- Apprehension: Fear or hesitation when running, jumping, or changing direction.
Early recognition of these symptoms is vital for effective treatment and recovery. If your child shows any of these signs, consult a healthcare professional for a thorough evaluation and appropriate care.
Doctor Examination for Patellar Dislocation
If your child’s kneecap (patella) has shifted back into place, it’s crucial to schedule a doctor’s visit as soon as possible. If the patella remains dislocated, seek immediate care at the emergency room to prevent further complications.
Medical History and Physical Examination
The diagnostic process begins with your child’s doctor taking a detailed medical history and conducting a physical examination. They will ask about how the injury happened and inquire about specific symptoms, such as pain or difficulty moving the knee.
During the examination, the doctor will assess:
- Range of Motion: To evaluate how well the knee moves.
- Tenderness: To identify any areas of discomfort.
- Knee Appearance: To check for swelling, deformity, or other visual abnormalities.
Diagnostic Tests
To confirm the diagnosis and develop a treatment plan, the doctor may recommend imaging tests:
- X-rays: These provide clear images of the bones in the knee, helping the doctor identify structural issues, such as a shallow femoral groove, which could contribute to patellar instability.
- Magnetic Resonance Imaging (MRI): While usually unnecessary for diagnosing a dislocated patella, MRIs offer detailed images of the knee’s soft tissues, including ligaments and cartilage. The doctor may request an MRI if additional insights are needed.
In some cases, a dislocated patella may cause a fragment of bone or cartilage to dislodge or loosen. These fragments can be detected on X-rays or MRI scans and may require further attention.
Prompt examination and appropriate diagnostic measures are essential to ensure your child receives the most effective treatment and achieves a full recovery.
 In this X-ray of a bent knee taken from above, the patella is clearly out of alignment within the groove in the femur.
In this X-ray of a bent knee taken from above, the patella is clearly out of alignment within the groove in the femur.
Treatment Options for Patellar Dislocation in Children
Immediate Treatment
If your child’s kneecap remains dislocated, it is essential to seek emergency medical care.
- Reduction Procedure: The doctor may administer pain relief to relax the knee muscles before gently repositioning the patella back into place through a process known as reduction.
Nonsurgical Treatment
In many cases, nonsurgical methods are sufficient for managing a patellar dislocation:
- Immobilization: Your child may be advised to wear a knee brace for 3 to 4 weeks. This stabilizes the knee and supports the healing process.
- Weightbearing Precautions: To reduce pain and avoid strain on the knee, the use of crutches may be recommended for the first week or two following the injury.
- Physical Therapy: Once initial healing occurs, physical therapy plays a crucial role in recovery. Specific exercises target the thigh muscles, particularly the quadriceps, to strengthen the knee joint and enhance stability. Commitment to the rehabilitation program is vital for a successful recovery. Most children can resume light activities within 3 to 6 weeks, although full recovery may vary.
Patellar dislocations often leave the kneecap looser and more prone to future instability, especially if caused by structural irregularities in the knee. Regular exercises, such as cycling, can help strengthen the thigh muscles and reduce the risk of recurrence.
Surgical Treatment
Surgery may be necessary if:
- The patella dislocates repeatedly.
- The kneecap remains unstable despite nonsurgical interventions.
The surgical approach depends on the underlying cause of instability:
- Ligament Reconstruction: This procedure strengthens or reconstructs the ligaments responsible for holding the kneecap in place. It is often performed arthroscopically using a small camera and specialized instruments.
- Complex Surgery for Structural Issues: If repeated dislocations are caused by congenital or bone deformities, more intricate surgical techniques may be required.
Safe Return to Activities
Once the knee regains full motion and strength, your child’s doctor will determine when it is safe to resume regular activities. For more demanding sports, a gradual return may be necessary to prevent reinjury.
Your child’s comfort and readiness are equally important considerations for a successful return to physical activity. Ongoing exercises to maintain muscle strength will support long-term knee stability and reduce the likelihood of future dislocations.