Overview:
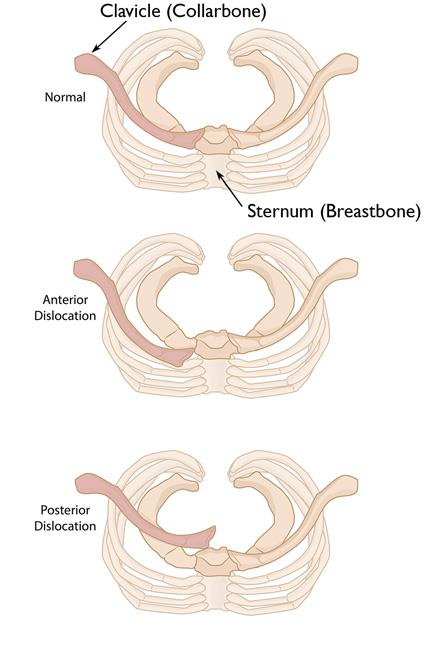
Sternoclavicular joint (SCJ) dislocations are rare but serious injuries that can be categorised into two main types: anterior and posterior. Anterior dislocations are more common and less dangerous. In contrast, posterior dislocations are less common but can be life-threatening because of their proximity to important structures like blood vessels and the windpipe. Accurate diagnosis and timely treatment are crucial to avoid severe complications.
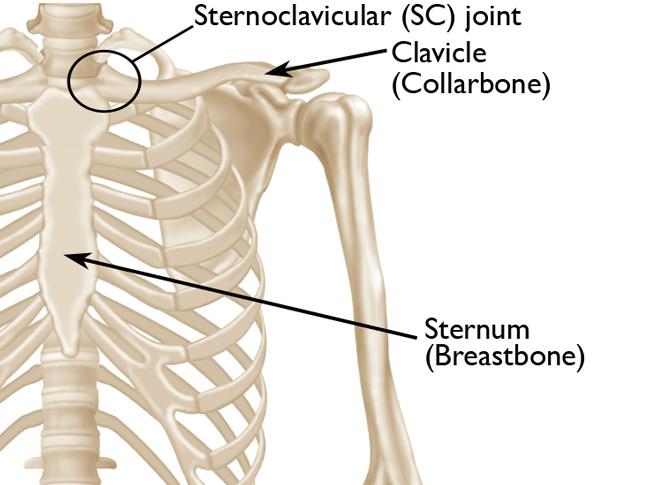
Understanding the Sternoclavicular Joint:
he SCJ is the joint where the collarbone (clavicle) meets the breastbone (sternum). It’s held together by several strong ligaments rather than relying on the bone shape for stability. The joint allows for a range of shoulder movements and plays a key role in lifting the arm.
Symptoms of SCJ Injuries:
- Anterior Dislocations: These present as a painful, noticeable bump near the sternum.
- Posterior Dislocations: These may not have a visible lump but can cause serious issues like difficulty breathing or swallowing due to pressure on nearby structures.
Causes of SCJ Injuries:
- High-energy trauma, such as car accidents or sports injuries.
- Direct impacts or falls onto the shoulder.
Diagnosing SCJ Injuries:
- Initial Imaging: Standard X-rays to get a basic view of the injury.
- Specialised Views: Specific X-ray techniques like the Serendipity view for better visualisation.
- CT Scans: Preferred for detailed images and to check for associated injuries.
- MRI and CT Angiography: Useful for assessing soft tissue and blood vessel involvement.
Types of SCJ Injuries:
- Direction of Displacement: Anterior, posterior, superior (upward), or inferior (downward).
- Ligament Damage: Classified by the extent of ligament injuries around the joint.
- Physeal Injuries: In younger patients (under 25), these injuries often mimic SCJ dislocations and need CT scans for accurate diagnosis
- (Top)Normal shoulder anatomy. (Center) In an anterior dislocation, the end of the clavicle is pushed forward, in front of the sternum. (Bottom) In a posterior dislocation, the end of the clavicle is pushed behind the sternum, toward several of the body’s vital structures.
Treatment Options:
- Non-Operative Management:
- For less severe injuries without dislocation (Grade I and II).
- Includes ice, immobilization with a sling, and anti-inflammatory medications.
- Anterior dislocations often managed without surgery, possibly using a closed reduction technique within the first week post-injury.
- Operative Management:
- Required for posterior dislocations due to the risk of severe complications.
- Also needed for persistent instability in anterior dislocations.
- Surgical techniques include:
- Open Reduction: Realigning the joint through surgery.
- Ligament Reconstruction: Using tendon grafts to repair the ligaments.
- Medial Clavicle Resection: Removing part of the collarbone if necessary.
- Figure-of-8 Reconstruction: Using either autografts (patient’s own tissue) or synthetic ligaments for the most reliable stability.
Key Takeaways:
- Early and Accurate Diagnosis: It is crucial to prevent complications, especially in posterior dislocations.
- Conservative Management: Effective for most anterior dislocations and non-displaced physeal injuries.
- Surgical Intervention: Necessary for unstable injuries, posterior dislocations, and cases with persistent instability.
- Team Approach: Collaboration with cardiothoracic surgeons during surgery can help manage potential complications.
Conclusion:
Sternoclavicular joint injuries, though rare, require careful management due to the potential for serious complications. Anterior dislocations are more common and typically managed without surgery, while posterior dislocations need prompt surgical intervention. Advances in imaging and surgical techniques have improved outcomes, highlighting the importance of personalised treatment strategies based on the specific type and severity of the dislocation.