Introduction:
Mucous cysts are small, fluid-filled sacs that commonly develop on the fingers, particularly in individuals aged 50 to 70. These cysts are often linked to osteoarthritis (OA) and typically form between the last joint of the finger and the base of the fingernail. If a mucous cyst is not causing pain or at risk of rupturing, it generally does not require treatment. However, even surgical removal of the cyst may not completely relieve discomfort if OA is the root cause of the pain.
This guide aims to provide insights into:
- The specific areas of the finger affected by mucous cysts
- How medical professionals diagnose this condition
- The available treatment options for mucous cysts
Anatomy
Which Part of the Finger is Affected?
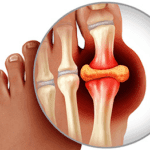
The fingers are composed of small bones known as phalanges. Each finger contains three phalanges, separated by two interphalangeal (IP) joints. The joint nearest to the knuckle is referred to as the proximal IP joint (PIP joint), while the joint ne
Ligaments, which are strong bands of connective tissue, link the bones and stabilize each finger joint. These ligaments form the joint capsule, a watertight sac encasing the joint. The surfaces of the joint are covered with articular cartilage, a smooth, spongy material that facilitates effortless movement between the joint surfaces. When this cartilage deteriorates, it leads to osteoarthritis (OA).
A mucous cyst is a specific type of ganglion, characterized as a small, harmless sac filled with a clear, sticky fluid composed of naturally occurring body chemicals. This cyst is connected to the DIP joint by a tissue stalk. Typically, only one mucous cyst develops, although an additional hidden (occult) cyst may occasionally form closer to the joint.
Causes :
What Causes Mucous Cysts?
Mucous cysts are most commonly associated with osteoarthritis (OA), though the exact reason for their development remains unclear.
The precise mechanism behind mucous cyst formation is not fully understood. One prevailing theory suggests that these cysts arise due to the degeneration of connective tissue. Collagen, a key protein in connective tissue, may break down and accumulate in small pools, eventually forming cysts. Additionally, it is believed that joint fluid flows into the cyst but does not return to the joint, contributing to its growth.
Symptoms:
What Are the Symptoms of a Mucous Cyst?
A mucous cyst usually appears as a visible lump just beneath the skin on the finger and may cause discomfort or pain. In some cases, you might observe a groove in the fingernail located directly above the cyst. This groove forms due to pressure exerted by the cyst on the nailbed. Additionally, the skin covering the cyst may become thinner over time.
Diagnosis :
How Is a Mucous Cyst Diagnosed?
To diagnose a mucous cyst, your doctor will review your medical history and carefully examine your fingers. They may also recommend an X-ray of the DIP joint. The X-ray can reveal signs of osteoarthritis (OA), such as bone spurs, narrowing of the joint space, and hardening of the subchondral bone—the layer of bone located just beneath the joint’s articular cartilage. Additionally, the presence of Heberden’s nodes may be noted. These nodes are bony bumps formed by bone spurs that develop in the finger joint as a result of OA.
Treatment
What can be done for the condition?
Treatment for mucous cysts may be either nonsurgical or surgical. The relative risks and benefits of any mucous cyst treatment should be considered carefully