Arthritis refers to the inflammation of one or more joints, commonly presenting with pain, swelling, and stiffness. While this condition can affect any joint in the body, it is particularly prevalent in the knee.
Knee arthritis often interferes with daily activities such as walking or climbing stairs, making it a leading cause of disability and lost productivity for many individuals.
Osteoarthritis and rheumatoid arthritis are the most prevalent forms, but the condition encompasses over 100 distinct types. Although arthritis primarily impacts adults, certain types can also affect children.
While there is currently no cure for arthritis, numerous treatment options are available to alleviate symptoms, reduce pain, and support an active lifestyle.
Anatomy of the Knee
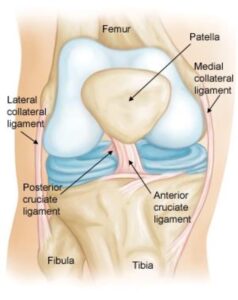
The knee is the largest and strongest joint in the human body, consisting of three main components: the lower end of the femur (thighbone), the upper end of the tibia (shinbone), and the patella (kneecap). These bones are covered with a layer of articular cartilage, a smooth, slippery material that cushions and protects the bones while allowing seamless movement as you bend or straighten your knee.
Within the knee joint, two wedge-shaped pieces of cartilage called the menisci serve as “shock absorbers” between the femur and tibia. These tough, rubbery structures provide cushioning and enhance joint stability.
The knee joint is enclosed by the synovial membrane, a thin layer that secretes synovial fluid. This fluid plays a crucial role in lubricating the cartilage and minimizing friction during movement.
Normal knee anatomy. The knee is made up of bones, cartilage, ligaments, and tendons.
Description of Knee Arthritis
The three primary types of arthritis that commonly affect the knee are osteoarthritis, rheumatoid arthritis, and post-traumatic arthritis.
Osteoarthritis
Osteoarthritis is the most prevalent form of knee arthritis and is often referred to as a “wear-and-tear” condition. While it typically affects individuals aged 50 and older, it can also occur in younger people.
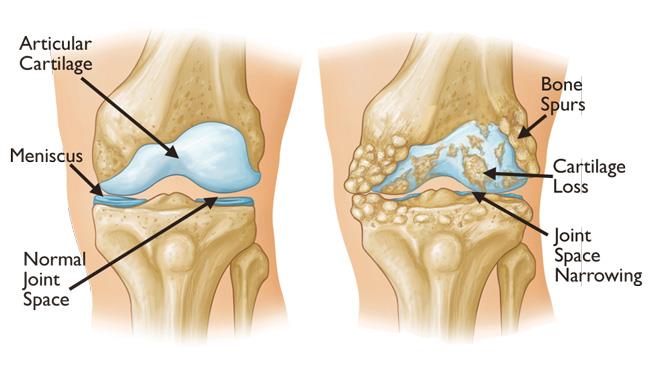
In osteoarthritis, the cartilage that cushions the knee joint gradually deteriorates. As the cartilage breaks down, it becomes rough and uneven, reducing the protective space between the bones. This can lead to bone-on-bone contact and the formation of painful bone spurs.
The progression of osteoarthritis is typically slow, with pain and discomfort intensifying over time
Osteoarthritis often results in bone rubbing on bone. Bone spurs are a common feature of this form of arthritis.
Rheumatoid Arthritis
Rheumatoid arthritis is a chronic autoimmune condition that affects multiple joints throughout the body, including the knees. It is typically symmetrical, meaning it often impacts the same joint on both sides.
In this disease, the synovial membrane surrounding the knee joint becomes inflamed, leading to pain, swelling, and stiffness in the affected area.
As an autoimmune disorder, rheumatoid arthritis occurs when the immune system mistakenly attacks the body’s own tissues. This results in damage to cartilage, ligaments, and even bone, contributing to the progressive weakening of the knee joint.
Post-Traumatic Arthritis
Post-traumatic arthritis is a type of arthritis that develops following an injury to the knee. This can occur after events like fractures that damage the joint surface or injuries to the meniscus and ligaments. Such injuries can destabilize the knee joint, leading to increased wear and tear over time and eventually causing arthritis.
Symptoms of Knee Arthritis
Arthritis in the knee can result in pain and inflammation that typically worsens gradually, although sudden onset is also possible. Common symptoms include:
- Stiffness and swelling: Difficulty bending or straightening the knee.
- Morning stiffness or post-rest pain: Symptoms often worsen after periods of inactivity, such as in the morning or after sitting.
- Activity-induced pain: Vigorous activities can cause symptoms to flare up.
- Locking or grinding: Loose cartilage fragments may interfere with joint movement, causing the knee to lock, creak, or grind (a condition known as crepitus).
- Weakness or instability: Pain may cause the knee to feel weak or prone to buckling.
- Weather sensitivity: Many people with arthritis notice increased joint pain with weather changes.
Doctor Examination
During a consultation, the doctor will review your symptoms and medical history, perform a physical examination, and may recommend diagnostic imaging or laboratory tests for further evaluation.
Physical Examination
The physical exam will include an assessment of:
- Swelling, warmth, or redness around the joint.
- Tenderness and range of motion (both assisted and self-directed).
- Joint stability and presence of crepitus during movement.
- Pain when bearing weight on the knee.
- Gait issues or other movement irregularities.
- Signs of involvement in other joints, which may indicate rheumatoid arthritis.
Imaging Tests
- X-rays: X-rays are used to evaluate bone structures and identify arthritis-specific changes, such as joint space narrowing, bone changes, or bone spur formation.
- Advanced imaging: In some cases, magnetic resonance imaging (MRI) or computed tomography (CT) scans may be needed to assess the condition of soft tissues and bones in greater detail.
By combining clinical evaluations and imaging studies, doctors can provide an accurate diagnosis and tailor treatment plans for effective management.
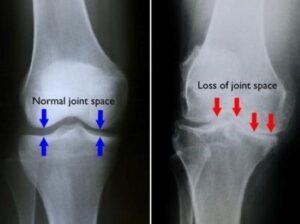 (Left) In this X-ray of a normal knee, the space between the bones indicates healthy cartilage (arrows). (Right) This X-ray of an arthritic knee shows severe loss of joint space.
(Left) In this X-ray of a normal knee, the space between the bones indicates healthy cartilage (arrows). (Right) This X-ray of an arthritic knee shows severe loss of joint space.
Laboratory Tests
To accurately identify the type of arthritis affecting your knee, your doctor may suggest blood tests. These tests are particularly useful in diagnosing certain forms of arthritis, such as rheumatoid arthritis, by identifying specific markers associated with the disease. Blood tests play a crucial role in confirming the diagnosis and guiding the appropriate treatment plan.
Treatment Overview
Although there is no cure for arthritis, a variety of treatment options can help alleviate pain, improve joint function, and enhance the quality of life for those affected by knee arthritis.
Nonsurgical Treatments
Lifestyle Modifications
Making certain adjustments to your daily routine can help protect the knee joint and slow arthritis progression:
- Limit activities that exacerbate knee pain, such as climbing stairs.
- Engage in low-impact exercises like swimming, cycling, or yoga to improve joint function and reduce stress on the knee.
- Incorporate balance, agility, and coordination exercises to enhance mobility and walking speed.
- Losing weight can significantly reduce pressure on the knee joint, resulting in decreased pain and improved functionality.
Physical Therapy
A tailored physical therapy program can strengthen the leg muscles, enhance flexibility, and improve range of motion. A physical therapist can design exercises to suit your specific needs.
Assistive Devices
- Braces:
- “Unloader” braces shift weight away from the affected part of the knee.
- “Support” braces provide overall stability.
- Canes and knee sleeves can also offer support. However, shoe wedges are not recommended for knee arthritis relief.
Other Remedies
Applying heat or ice packs and wearing elastic bandages may alleviate discomfort.
Medications
Several medications can manage knee arthritis effectively:
- Over-the-counter (OTC) pain relievers: Non-narcotic options like acetaminophen help reduce mild arthritis pain.
- Nonsteroidal anti-inflammatory drugs (NSAIDs): Available as OTC or prescription (e.g., ibuprofen or naproxen), these can alleviate pain and improve function. Topical NSAIDs are strongly recommended if oral options are not suitable. However, NSAIDs should be used cautiously in individuals with conditions like heart disease or kidney issues.
- COX-2 inhibitors: These NSAIDs (e.g., celecoxib) may reduce gastrointestinal side effects but should not be combined with other NSAIDs.
- Corticosteroid injections: These powerful anti-inflammatory medications provide temporary pain relief. However, repeated use can lead to joint damage, and injections should be limited to three or four per year.
- DMARDs: Disease-modifying anti-rheumatic drugs (e.g., methotrexate, sulfasalazine) and biologics (e.g., etanercept, adalimumab) are effective in managing rheumatoid arthritis.
- Supplements: Glucosamine and chondroitin sulfate may provide pain relief, but their effectiveness in slowing arthritis progression remains unproven. Always consult your doctor before using supplements.
Alternative Therapies
- Acupuncture: May relieve arthritis pain; ensure the practitioner is certified.
- Magnetic Pulse Therapy: Painless but lacks conclusive evidence of effectiveness.
- Biologic Treatments: Platelet-rich plasma (PRP) and stem cell injections show promise in reducing inflammation and potentially regenerating joint tissue, though further research is needed.
Surgical Treatments
When nonsurgical treatments fail to relieve pain or improve function, surgical options may be recommended.
Arthroscopy
This minimally invasive procedure uses small incisions to treat joint problems. It may be used in cases where arthritis is accompanied by a degenerative meniscal tear.
Cartilage Grafting
Healthy cartilage from another part of the knee or a tissue bank can be used to repair localized cartilage damage, primarily in younger patients.
Synovectomy
For rheumatoid arthritis, the inflamed synovial lining is surgically removed to reduce swelling and pain.
Osteotomy
This procedure involves reshaping the tibia or femur to relieve pressure on the knee joint. It is particularly effective for early-stage osteoarthritis affecting one side of the knee.
Knee Replacement (Arthroplasty)
- Total Knee Replacement: Damaged cartilage and bone are replaced with metal or plastic components to restore joint function.
- Partial Knee Replacement: Focuses on replacing only the affected portion of the knee.
Each surgical option comes with risks, which your doctor will discuss with you prior to the procedure to ensure an informed decision.
 (Left) A partial knee replacement is an option when damage is limited to just one part of the knee. (Right) A total knee replacement prosthesis.
(Left) A partial knee replacement is an option when damage is limited to just one part of the knee. (Right) A total knee replacement prosthesis.
Recovery After Knee Arthritis Surgery
Recovery following knee arthritis surgery varies depending on the procedure performed. Both recovery time and rehabilitation requirements are influenced by the specific surgical approach.
To restore knee strength and improve range of motion, your doctor may recommend a physical therapy program. Based on the surgery, you might also need to use a knee brace, crutches, or a cane during the initial recovery phase.
For most patients, surgery significantly reduces pain and enhances the ability to perform everyday tasks with greater ease.
To support effective management of knee osteoarthritis, both nonsurgically and surgically, the American Academy of Orthopaedic Surgeons has developed evidence-based guidelines to assist healthcare providers in delivering optimal care.