Introduction
Kienböck’s disease is a rare condition that affects the wrist, where one of the small carpal bones—specifically the lunate—loses its blood supply and begins to deteriorate. This condition leads to pain, stiffness, and restricted wrist movement. As the disease progresses, the lunate bone collapses, disrupting the alignment of surrounding wrist bones. Over time, these changes contribute to degenerative joint disease and osteoarthritis. While the exact cause of Kienböck’s disease remains unclear, various treatment options exist to manage symptoms and preserve wrist function.
This guide will provide insight into:
- The development and progression of Kienböck’s disease
- Diagnostic methods used by healthcare professionals
- Available treatment approaches
Anatomy of the Wrist
How Does the Wrist Function?
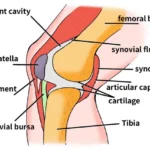
The wrist joint is one of the most intricate structures in the human body. It consists of multiple interconnected bones and joints, allowing for a wide range of motion and dexterity essential for hand function. While the wrist needs to be highly mobile to facilitate fine motor movements, it must also provide stability and strength for tasks requiring a firm grip.
The wrist comprises eight small carpal bones, collectively forming a complex joint system. Among these bones, the lunate plays a crucial role in wrist mobility. In Kienböck’s disease, this bone becomes compromised due to a lack of blood supply, ultimately affecting overall wrist function.
Causes of Kienböck’s Disease
Why Does Kienböck’s Disease Occur?
The exact cause of Kienböck’s disease remains uncertain, but several contributing factors have been identified. In most cases, a wrist injury—such as a sprain or repeated trauma—precedes the condition. However, injury alone does not directly cause the disease.
One of the key factors is the blood supply to the lunate bone. Some bones in the body naturally have fewer blood vessels, and the lunate is among them. A restricted blood supply makes it more vulnerable to damage, particularly after an injury. If the blood vessels supplying the lunate are compromised, either due to trauma or an anatomical variation, the risk of developing Kienböck’s disease increases.
Additionally, the surrounding bones may contribute to the disease. The ulna, one of the two forearm bones, plays a role—especially if it is shorter than the radius. When this occurs, the lunate absorbs excessive force during activities requiring heavy gripping. Over time, these repeated stresses may contribute to blood vessel damage or direct injury to the lunate, increasing the likelihood of osteonecrosis.
Kienböck’s disease has also been observed in individuals with medical conditions that affect small blood vessels, suggesting that systemic factors might influence its development. Regardless of the cause, the lunate undergoes osteonecrosis, a condition where the bone deteriorates due to inadequate blood flow.
Symptoms of Kienböck’s Disease
What Are the Signs and Symptoms?
The most common symptoms of Kienböck’s disease include:
- Wrist pain that may range from mild discomfort to persistent pain
- Limited wrist movement, with difficulty in bending or rotating the wrist
- Pain that worsens over time, often starting only after heavy wrist use but gradually becoming more constant
- Swelling around the wrist, particularly on the back side near the lunate
- Tenderness over the affected area, making wrist movement painful
- Weak grip strength, making it harder to grasp objects
Many individuals experience symptoms for months or even years before seeking medical attention. In most cases, patients report a previous wrist injury or a history of repetitive wrist use. Kienböck’s disease is most commonly diagnosed in men between the ages of 20 and 40 and rarely affects both wrists simultaneously.
Diagnosis of Kienböck’s Disease
How Is Kienböck’s Disease Diagnosed?
To diagnose Kienböck’s disease, a doctor will first take a detailed medical history and perform a physical examination of the wrist.
Imaging Tests
Several imaging techniques are used to confirm the diagnosis and determine the severity of the disease:
- X-rays: Help assess bone changes and determine the disease stage.
- Magnetic Resonance Imaging (MRI): Provides highly detailed images of soft tissues and bones. MRI is particularly useful when there is uncertainty about whether the lunate bone has lost its blood supply, as it can accurately detect changes in blood flow.
In most cases, these imaging tests provide a clear diagnosis, and additional testing is not required.
Treatment for Kienböck’s Disease
What Are the Treatment Options?
Kienböck’s disease progresses slowly, often over several years. To determine the most appropriate treatment, hand surgeons classify the disease into four stages based on severity.
Stages of Kienböck’s Disease
- Stage 1: The lunate loses its blood supply, and fractures may develop.
- Stage 2: The bone hardens (sclerosis) due to ongoing blood supply loss.
- Stage 3: The lunate collapses, sometimes breaking into multiple pieces and shifting out of position.
- Stage 4: The disease leads to wrist osteoarthritis, damaging surrounding bones.
The choice of treatment depends on the stage of progression.
Non-Surgical Treatment
For early-stage Kienböck’s disease (Stage 1), non-surgical management is often the first approach.
- Immobilization: Doctors may recommend wearing a cast for up to three months to allow the wrist to heal.
- Spontaneous Recovery: In some cases, blood supply may return on its own, especially if the patient has transient osteonecrosis, a temporary condition that mimics Kienböck’s disease following injury.
If symptoms persist or worsen, surgical intervention may be necessary.
Surgical Treatment for Kienböck’s Disease
1. Revascularization Surgery (Restoring Blood Flow)
For Stage 2 or 3 Kienböck’s disease, when immobilization is ineffective, surgical revascularization may be attempted.
- In this procedure, a small section of bone and blood vessels is taken from another part of the body and grafted onto the lunate.
- The goal is to restore circulation and slow disease progression.
- However, this is a relatively new technique, and its success varies.
2. Arthroscopy & Lunate Fusion
- Minimally invasive technique using an arthroscope (a thin, camera-equipped instrument).
- The lunate is fused to an adjacent carpal bone to stabilize the wrist.
- This procedure helps limit movement that could worsen the condition but does not necessarily restore blood flow.
3. Lunate Decompression
- Aims to relieve pressure on the lunate, potentially allowing for healing.
- Radial Shortening Osteotomy: A small segment of the radius is removed to reduce stress on the lunate.
- Capitate Shortening (Almquist Procedure): Shortens an adjacent carpal bone to distribute pressure more evenly.
Both procedures help reduce strain on the lunate, potentially delaying disease progression.
4. Carpectomy (Bone Removal) for Late-Stage Disease
In Stage 4 Kienböck’s disease, when osteoarthritis has developed, proximal-row carpectomy may be performed.
- This involves removing the four bones in the wrist’s proximal row, including the collapsed lunate.
- The remaining wrist bones adjust their position, preserving some range of motion.
- Advantage: Allows for continued wrist flexibility, making it a good option for musicians or individuals needing fine motor control.
5. Wrist Fusion (For Severe Cases)
- In advanced cases where the wrist joint is severely arthritic, wrist fusion may be recommended.
- While this procedure eliminates pain, it limits wrist mobility.
- This option is best suited for patients who require strength over flexibility.
Final Thoughts
Kienböck’s disease is a progressive wrist condition that requires early diagnosis and treatment to prevent long-term complications. While mild cases may improve with non-surgical methods, advanced stages often require surgical intervention. The best treatment approach depends on disease severity, wrist anatomy, and patient needs.
Wrist Fusion for Kienböck’s Disease
In advanced cases where severe wrist arthritis has developed, wrist fusion (arthrodesis) may be recommended. This procedure involves fusing all the wrist bones together to form a single, solid bone. While this eliminates pain, it also prevents wrist flexion and extension, resulting in a stiff wrist. However, forearm rotation (turning the palm up and down) remains unaffected.
Wrist fusion is an ideal option for individuals who require strength over flexibility, such as those engaged in manual labor or physically demanding tasks.
Rehabilitation After Treatment
Recovery from Nonsurgical Treatment
If the lunate bone remains well-aligned, doctors may opt for immobilization in a cast for up to 12 weeks. This period allows blood supply to return and promotes natural healing.
Once the doctor confirms healing, the cast is removed. However, stiffness and weakness are common due to prolonged immobilization. To restore wrist strength and mobility, physical or occupational therapy is often recommended for 4 to 6 weeks.
Recovery After Surgery
Following surgery, patients are typically placed in a wrist splint for approximately 12 weeks to support healing. During this time, the surgeon will perform regular X-rays to monitor bone healing. Once healing progresses, a structured rehabilitation program can begin.
Post-Surgical Rehabilitation Timeline
- First phase (1–4 weeks): Focuses on pain and swelling management.
- Intermediate phase (4–8 weeks): Introduces strengthening exercises to improve muscle stability around the wrist.
- Final phase (8–12 weeks): Incorporates exercises for fine motor control and dexterity, ensuring optimal hand function.
Patients will also receive ergonomic tips and movement modifications to minimize strain on the wrist while performing daily activities.
Final Thoughts
Recovery from Kienböck’s disease treatment—whether nonsurgical or surgical—requires patience and rehabilitation to restore wrist function. While wrist fusion sacrifices mobility, it provides long-term pain relief and stability. Working closely with a hand therapist or rehabilitation specialist can significantly improve outcomes and enhance wrist functionality.