Introduction
Knee pain and tenderness near the lower kneecap in children and adolescents can be a sign of conditions such as jumper’s knee. This injury is especially common among young athletes participating in sports that involve frequent kicking, jumping, or running. The repetitive strain on the tendon that spans the front of the kneecap can lead to significant discomfort.
In certain cases, the issue is linked to the bone growth center at the lower tip of the kneecap—a condition known as Sinding-Larsen-Johansson disorder. This disorder typically emerges during growth spurts, when the developing bone is more vulnerable to stress. Although it may cause pain and tenderness in the front of the knee, Sinding-Larsen-Johansson disorder is generally mild and tends to resolve as the child matures.
This comprehensive guide is designed to help you understand:
• Knee Anatomy: Identify the specific structures of the knee involved in these conditions.
• Causes: Explore the factors that contribute to these types of knee injuries.
• Treatment Options: Review the available strategies for managing pain and promoting recovery.
By delving into these topics, parents, caregivers, and young athletes can better understand and address sports-related knee injuries, ensuring a safe and healthy growth process.
Anatomy
Which Part of the Knee Is Involved?
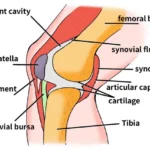
Jumper’s knee primarily affects the patellar tendon, a crucial structure in the knee. This tendon connects the robust quadriceps muscle at the front of the thigh to the shinbone (tibia), playing a vital role in leg movement and stability. The patellar tendon travels over the anterior surface of the kneecap (patella), anchoring at two key points:
- Upper Attachment: The tendon attaches to the bottom tip of the kneecap, known as the inferior pole of the patella.
- Lower Attachment: It connects to the tibia at a small bony prominence called the tibial tuberosity.
Understanding this anatomical structure is essential for recognizing how repetitive strain in sports can lead to conditions like jumper’s knee, affecting performance and comfort.
Causes
How Jumper’s Knee and Related Disorders Develop
Jumper’s knee typically arises from repetitive stress and overuse of the patellar tendon. Young athletes involved in sports that require frequent squatting, jumping, and rapid deceleration are especially susceptible. Here’s how the condition unfolds:
Overuse and Eccentric Contraction:
During activities like landing from a jump or performing a deep squat, the quadriceps muscle works eccentrically—it lengthens while contracting—to slow down the body and protect the knee. This intense muscle action puts excessive tension on the patellar tendon, causing microtrauma to its fibers. With repeated stress, the tendon becomes inflamed and painful, leading to jumper’s knee.Abnormal Lower Limb Alignment:
Structural issues such as knock-knees or flat feet can alter the natural alignment of the leg. These misalignments increase the Q-angle (the angle between the quadriceps muscle and the patellar tendon), which adds extra strain on the tendon. A larger Q-angle not only heightens the risk of developing jumper’s knee but also places abnormal tension on the bone growth plate at the inferior pole of the patella, making Sinding-Larsen-Johansson disorder more likely. Additionally, a high-riding kneecap—known as patella alta—may further contribute to these conditions.Growth-Related Factors:
In active children, rapid growth can create a discrepancy between bone development and tendon length. During growth spurts, the patellar tendon might not lengthen at the same pace as the lower leg, resulting in increased tension at the bottom tip of the kneecap. This excess pull, especially when combined with heavy or repetitive sports activity, can disrupt normal bone development. When this occurs at the inferior pole of the patella, it is recognized as Sinding-Larsen-Johansson disorder.
This condition is part of a broader group of bone development disorders known as osteochondroses, where growth plates (the centers where cartilage gradually transforms into bone) are affected. Children with one type of bone development issue, such as Sinding-Larsen-Johansson disorder, may also be at risk for related conditions like Osgood-Schlatter lesion, which involves the attachment of the patellar tendon to the tibial tuberosity.
Understanding these causes—from repetitive overuse and eccentric muscle actions to biomechanical misalignments and growth-related challenges—can help parents, coaches, and young athletes recognize early signs and take appropriate steps toward prevention and treatment.
Symptoms
Recognizing Knee Pain in Young Athletes
Jumper’s knee typically presents as localized pain and tenderness along the patellar tendon—just below the kneecap. This discomfort is often accompanied by mild swelling and can be particularly pronounced when kneeling. Activities that engage the quadriceps in an eccentric contraction, such as squatting, jumping, or descending stairs, usually exacerbate the pain.
In cases of Sinding-Larsen-Johansson disorder, the pain is generally experienced at the upper part of the kneecap where the quadriceps meets the patellar tendon. Affected children might also report a feeling of tightness, especially when attempting to fully bend the knee.
Diagnosis
Clinical Examination and Imaging Techniques
Diagnosing jumper’s knee starts with a comprehensive history and physical evaluation. Doctors gather details about the child’s age, activity level, and symptom duration while performing a targeted examination that includes:
- Palpation: Pressing around the kneecap and along the patellar tendon to identify tender areas.
- Comparative Assessment: Evaluating differences between the affected knee and its healthy counterpart.
- Resisted Knee Extension: Asking the patient to extend the knee against resistance, which stresses the quadriceps and patellar tendon. Pain during this maneuver is a key indicator.
For suspected Sinding-Larsen-Johansson disorder, or when trauma is involved, additional imaging may be necessary:
- X-rays: A lateral view of the knee can reveal small bone fragments, calcifications, or irregularities at the inferior pole of the patella. This imaging is also crucial for ruling out patellar fractures.
- Magnetic Resonance Imaging (MRI): An MRI provides a detailed look at the patellar tendon, identifying subtle calcifications, inflammation, and swelling that might not be visible on an X-ray.
Treatment Options
Conservative Management and Surgical Interventions
Non-Surgical Management
Conservative treatment is often effective for managing jumper’s knee and Sinding-Larsen-Johansson disorder, especially in young athletes whose bones are still developing:
- Activity Modification: Temporarily reducing or pausing sports activities helps control pain and inflammation without long-term activity restrictions.
- Rest and Natural Healing: In growth-related cases (Sinding-Larsen-Johansson disorder), symptoms frequently resolve naturally over one to two years as the growth plates in the inferior pole of the patella fuse.
- Medications: Anti-inflammatory drugs can be prescribed to alleviate swelling and discomfort.
- Supportive Devices: Knee straps or sleeves may be used to provide additional support and reduce pain during movement.
- Physical Therapy: A structured rehabilitation program can be vital. Treatments may include:
- Modalities: Ice, heat, or ultrasound therapies to manage inflammation.
- Exercise Programs: Stretching and strengthening exercises to enhance flexibility, muscle balance, and proper knee alignment.
- Orthotics: Custom shoe inserts designed to correct flat feet or knock-kneed posture and optimize lower limb mechanics.
It is important to note that while cortisone injections are used for other inflammatory conditions, they are generally avoided in jumper’s knee due to inconsistent benefits and an increased risk of patellar tendon rupture.
Surgical Intervention
Surgery is rarely needed and is considered only when non-surgical measures fail to relieve symptoms—typically in cases that involve persistent tendon damage rather than issues with the growth plate. Surgical options may include:
- Tendon Debridement: A minimally invasive procedure where a small incision is made below the kneecap to expose and remove inflamed or damaged tissue from the surface of the patellar tendon.
- Stimulating Healing: In some cases, small drill holes are created in the inferior pole of the patella to induce a healing response via controlled bleeding.
This targeted surgical approach is designed to alleviate pain and restore normal tendon function, with most patients experiencing significant improvement post-procedure.
By understanding the symptoms, diagnostic methods, and treatment options for jumper’s knee and Sinding-Larsen-Johansson disorder, parents, coaches, and young athletes can take proactive steps toward effective management and a safe return to sports.
Rehabilitation
What to Expect from Treatment
Effective rehabilitation for jumper’s knee and Sinding-Larsen-Johansson disorder focuses on reducing pain, managing inflammation, and gradually restoring function. Treatment options vary based on whether the approach is non-surgical or follows surgery.
Non-Surgical Rehabilitation
Non-surgical strategies aim to alleviate discomfort and correct underlying issues through a combination of therapies and lifestyle adjustments. Key components include:
Pain and Inflammation Management:
- Modalities: Techniques such as ice, heat, and ultrasound help control swelling and ease pain.
- Activity Modification: Patients are advised to temporarily avoid high-impact activities, including intense sports, to prevent further stress on the knee.
Physical Therapy:
- Flexibility Training: Stretching exercises for the hamstrings and quadriceps reduce tension in the patellar tendon at its attachment on the kneecap.
- Strengthening Exercises: Targeted workouts improve muscle balance, supporting proper knee movement and alignment during activity.
- Biomechanical Correction: Therapists may introduce posture exercises and recommend custom orthotics to enhance leg alignment and decrease knee strain.
In cases of Sinding-Larsen-Johansson disorder, where the bone growth plate is involved, non-surgical treatments typically offer short-term relief. As the growth plates gradually fuse over time, symptoms tend to diminish, but the rehabilitation process itself may not fully “cure” the underlying condition.
Post-Surgery Recovery
When non-surgical methods are insufficient, surgical intervention might be necessary. The post-surgical rehabilitation process is carefully structured to promote healing and restore function:
Immediate Post-Operative Care:
- Hinged Knee Brace: Patients often wear a brace that allows controlled bending while limiting full extension of the quadriceps, protecting the healing tendon.
- Weight-Bearing Support: Crutches are typically recommended until the patient can comfortably bear weight without pain.
Follow-Up and Early Rehabilitation:
- Initial Check-Up: About 10 to 14 days after surgery, stitches are removed, and the patient begins gentle exercises to encourage knee mobility.
- Early Physical Therapy: The first phase focuses on managing post-operative pain and swelling, gradually progressing to exercises that improve range of motion and strengthen the quadriceps.
Gradual Return to Daily Activities:
- Activity Resumption: Patients are encouraged to slowly resume routine activities.
- Exercise Restrictions: Vigorous exercise should be avoided for at least six weeks after surgery, with high-level sports typically postponed for up to six months. This cautious timeline ensures that the knee regains full strength and stability before returning to demanding athletic activities.
By following a structured rehabilitation program, young athletes can expect a steady improvement in knee function, reduced pain, and a safe return to their sporting activities once their quadriceps strength and overall knee stability are restored.