Patients with advanced hip arthritis may consider two surgical options: traditional total hip replacement (arthroplasty) or hip resurfacing (hip resurfacing arthroplasty). While both are forms of hip replacement surgery, they differ significantly in procedure and application. Your orthopaedic surgeon will guide you in understanding these options and recommend the most suitable procedure for your condition.
Description
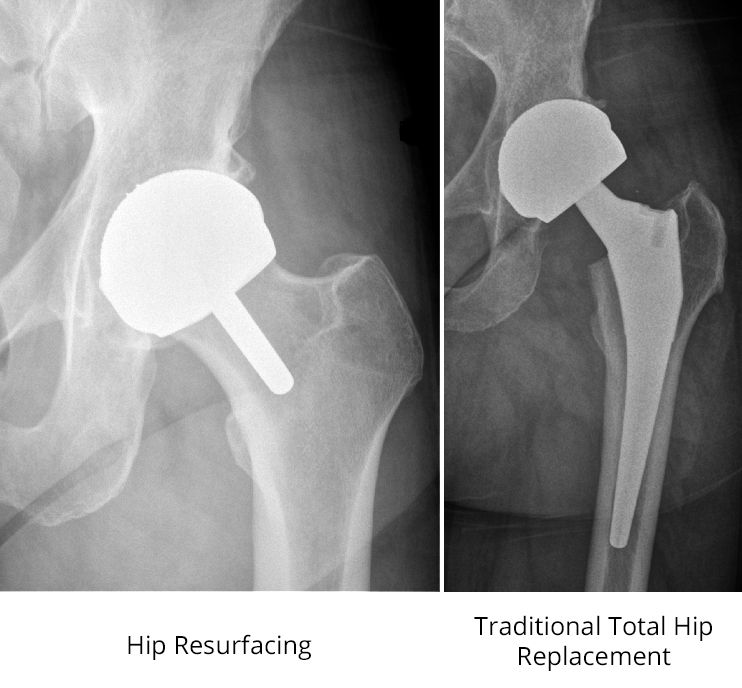
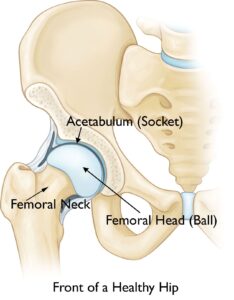
In a traditional total hip replacement, the femoral head (head of the thighbone) and the damaged socket (acetabulum) are completely removed and replaced with components made of metal, plastic, or ceramic.
In contrast, hip resurfacing preserves the femoral head. Instead of removing it, the surgeon trims and caps it with a smooth metal covering. As with total hip replacement, the damaged bone and cartilage in the socket are removed and replaced with a metal shell.
Let me know if you’d like further edits or additional sections!

(Left) In this X-ray of a hip resurfacing taken from the front, a metal cap now covers the femoral head, and a small stem is seen in the femoral neck. A metal socket is also in place. Unlike the traditional total hip replacement shown on the right, the femoral head and neck are not removed.
Advantages of Hip Resurfacing
The advantages of hip resurfacing over traditional total hip replacement remain a topic of debate among orthopaedic surgeons, and ongoing research seeks to provide clearer answers.
- Easier Revision Surgery:
Hip resurfacing may simplify revision surgery if the implant fails or wears out. Over time, implants can loosen or wear, often requiring replacement 15 to 20 years after the procedure. Because hip resurfacing preserves more bone in the femur than traditional hip replacement, many surgeons believe it is easier to replace failed implants in resurfaced hips. - Lower Risk of Hip Dislocation:
The larger ball size used in hip resurfacing more closely resembles the natural size of the hip joint, potentially reducing the risk of dislocation. However, this benefit is debated, as other factors like surgical technique and implant design also influence dislocation risk. - More Natural Walking Pattern:
Some studies suggest that patients experience a more natural walking pattern following hip resurfacing compared to traditional hip replacement. These differences are subtle and require specialized instruments to detect.
Disadvantages of Hip Resurfacing
- Femoral Neck Fracture:
A small percentage of hip resurfacing patients experience a fracture in the femoral neck, which often necessitates converting the hip resurfacing to a traditional hip replacement. This type of fracture does not occur in traditional hip replacements because the femoral neck is removed during the procedure. However, fractures around implants can still happen with traditional replacements. - Metal Ion Risks:
Hip resurfacing involves a metal ball moving within a metal socket, which can release tiny metal ions due to friction. These ions may cause:- Adverse Local Tissue Reaction: Pain and swelling in the surrounding tissues, potentially requiring revision surgery.
- Systemic Effects: Metal ions can enter the bloodstream, raising concerns about body-wide impacts.
As a result of these risks, hip resurfacing is less commonly performed today. However, metal-on-metal implants in some traditional hip replacements carry similar risks.
Consult Your Surgeon
Ask your doctor for detailed information about the benefits and risks of metal-on-metal implants and whether hip resurfacing is a suitable option for you.
Let me know if you’d like further adjustments or additional edits!
Candidates for Hip Resurfacing Surgery
Surgery may be recommended if advanced osteoarthritis significantly impacts your quality of life and nonsurgical treatments have not been effective.
Unlike traditional hip replacement, hip resurfacing is not suitable for everyone. Ideal candidates generally:
- Are younger (under 60 years old).
- Have larger body frames (often, but not exclusively, male).
- Possess strong, healthy bone.
Patients who are older, smaller-framed, female, or have weakened bone are at higher risk for complications such as femoral neck fractures. A thorough evaluation by your orthopaedic surgeon will determine your suitability for the procedure.
Your Surgery
Before Surgery
You will likely be admitted to the hospital on the day of surgery.
- Anesthesia Consultation: An anesthesiologist will review your medical history and discuss anesthesia options, which may include:
- General anesthesia (you are asleep).
- Regional anesthesia (you are awake, but numb from the waist down).
- Preoperative Preparation: Your surgeon will verify the surgical site by marking your hip with a marker before the procedure.
Surgical Procedure
Hip resurfacing surgery typically lasts 1.5 to 3 hours. During the operation:
- The surgeon makes an incision in the thigh to access the hip joint.
- The femoral head is dislocated and trimmed using specialized instruments.
- A metal cap is cemented over the prepared femoral head.
- The cartilage lining the hip socket is removed using a reamer.
- A metal cup is inserted into the socket and held in place by friction with the bone.
- The femoral head is repositioned, and the incision is closed.
After surgery, you will be monitored in a recovery room before being transferred to your hospital room.
Potential Complications
Like any surgical procedure, hip resurfacing carries certain risks, including:
- Infection: Preventative antibiotics are administered before and after surgery.
- Blood Clots: Blood thinners such as aspirin, warfarin, or rivaroxaban may be prescribed to reduce this risk.
- Nerve or Vessel Injury: Rare but possible during surgery.
- Femoral Neck Fracture: Specific to hip resurfacing.
- Dislocation: Less common compared to traditional hip replacement.
- Anesthesia Risks: Depend on your overall health.
Recovery
Hospital Stay and Early Mobility
- Most patients are discharged within 1 to 4 days.
- Weight-bearing on the operated leg may begin immediately, depending on your surgeon’s guidance and bone strength. Walkers, canes, or crutches may be required initially.
Pain Management
- You may experience pain and discomfort for several weeks post-surgery. Pain management may include:
- Opioids: Effective but should be used only as prescribed due to addiction risk.
- NSAIDs: Help reduce inflammation and pain.
- Local Anesthetics: May be used to control localized pain.
Physical Therapy and Follow-Up
- Physical therapy will be recommended to maintain range of motion and restore strength.
- Follow-up visits with your orthopaedic surgeon will monitor your recovery progress.
Return to Activities
- Most patients can resume daily activities within six weeks of surgery. Full recovery depends on individual progress and adherence to rehabilitation plans.
Let me know if you’d like further refinements or assistance with a meta description and SEO title!