What is a frozen shoulder?
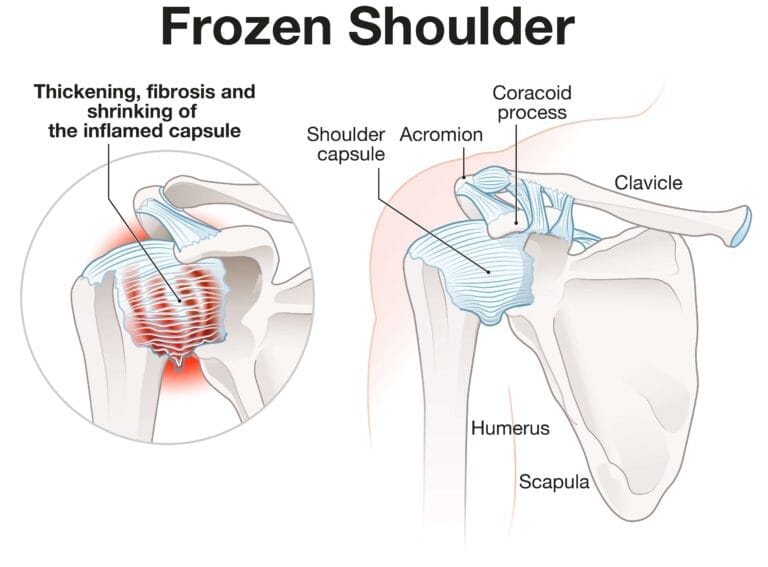
The shoulder joint is a ball and socket joint and the joint is surrounded by a structure called a joint capsule. The joint capsule is usually very mobile and flexible, moving freely as you move your arm. A frozen shoulder is when the joint capsule becomes inflamed, thickened and stiffer, subsequently causing pain and loss of movement at the shoulder joint. A frozen shoulder is also described as adhesive capsulitis, a stiff shoulder or a contracted shoulder.
Contributing factors and hallmark signs
• Aged between 40 to 60
• Diabetes
• Can happen after surgery or trauma
• Can come for no apparent reason
The hallmark signs of this condition are severe pain and being unable to move your shoulder – either on your own or with the help of someone else. It develops in three stages:
Causes and when to seek medical attention
Causes
The causes of frozen shoulder are not fully understood. There is no clear connection to arm dominance or occupation. A few factors may put you more at risk for developing a frozen shoulder.
Diabetes. Frozen shoulder occurs much more often in people with diabetes. The reason for this is not known. In addition, diabetic patients with frozen shoulder tend to have a greater degree of stiffness that continues for a long time before “thawing.”
Other diseases. Some additional medical problems associated with frozen shoulder include hypothyroidism, hyperthyroidism, Parkinson’s disease, and cardiac disease.
Immobilization. A frozen shoulder can develop after a shoulder has been immobilized for a period of time due to surgery, a fracture, or other injuries. Having patients move their shoulders soon after injury or surgery is one measure prescribed to prevent frozen shoulders.
When to seek medical attention?
• A new lump or bump around the shoulder
• Bruising or redness in and around the joint or new multiple joint swellings
• Feeling unwell with a temperature associated with the onset of this problem
• Loss of feeling and power in the arm
• Power loss associated with injury or a fall onto an outstretched hand• Unusual increase in breathlessness, or new persistent cough since the onset of this problem
Symptoms
Symptoms can vary in intensity both in the day and at night. The frozen shoulder usually starts with pain all around the shoulder and sometimes down the arm. The pain usually improves with time but the shoulder may feel stiffer and you cannot move the arm freely.
Simply, pain from frozen shoulder is usually dull or aching. It is typically worse early in the course of the disease and when you move your arm. The pain is usually located over the outer shoulder area and sometimes the upper arm.
What to expect
The frozen shoulder is a self-limiting condition, meaning it usually goes away by itself with time, the majority of symptoms resolve within two years, although occasionally last longer. Physiotherapy can help to speed this up with stretching exercises or other treatments, providing the pain is well controlled. Other treatments that may help the frozen shoulder include steroid injection and, in some cases, surgery may be required.
Treatment
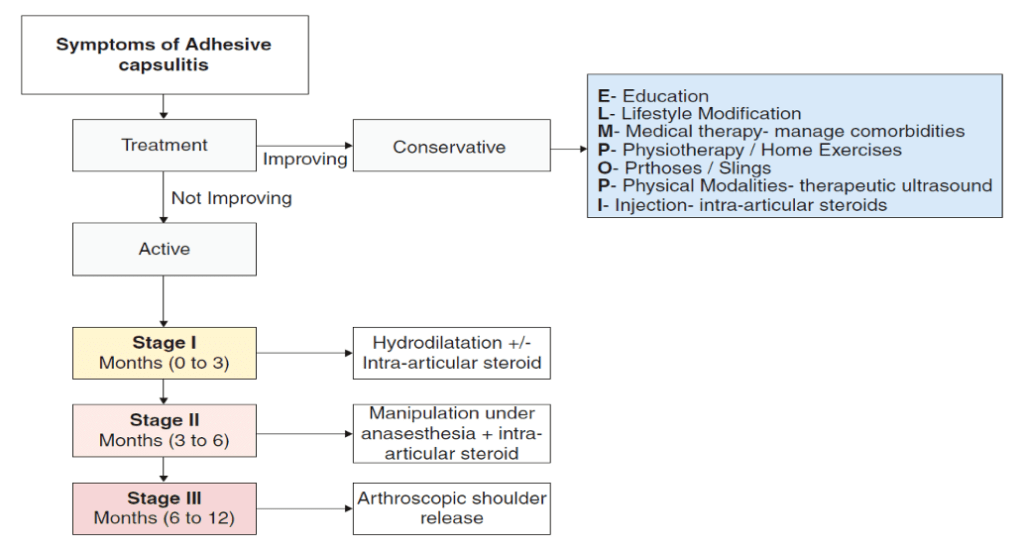
Frozen shoulder generally gets better over time, although it may take up to 3 years. The focus of treatment is to control pain and restore motion and strength through physical therapy.
Nonsurgical Treatment
Most people with frozen shoulder improve with relatively simple treatments to control pain and restore motion.
Non-steroidal anti-inflammatory medicines. Drugs like aspirin and ibuprofen reduce pain and swelling.
Steroid injections. Cortisone is a powerful anti-inflammatory medicine that is injected directly into your shoulder joint.
Hydrodilatation. If your symptoms are not relieved by other nonsurgical methods, your doctor may recommend hydrodilatation. This procedure involves gently injecting a large volume of sterile fluid into the shoulder joint to expand and stretch the shoulder joint capsule. Hydrodilatation is conducted by a radiologist who uses imaging to guide the placement of fluid.
Hydrodilatation or hydraulic arthrographic capsular distension is a medical treatment for adhesive capsulitis of the shoulder. Risk of complications is low. Whether the treatment is successful is known after a couple of weeks. The procedure is performed under imaging guidance. Hydrodilatation is felt to provide benefit via two mechanisms: manual stretching of the capsule and thus disruption of adhesions which are characteristic of adhesive capsulitis, and; increasing the surface area of the capsule then the introduction of cortisone provides a potent anti-inflammatory effect and thus prevents further adhesion recurrence.
Physiotherapy. Specific exercises will help restore motion. These may be done under the supervision of a physical therapist or via a home program. Therapy includes stretching or range of motion exercises for the shoulder. Sometimes heat is used to help loosen the shoulder up before stretching. Below are examples of some of the exercises that might be recommended.
- External rotation — passive stretch. Stand in a doorway and bend your affected arm’s elbow to 90 degrees to reach the doorjamb. Keep your hand in place and rotate your body as shown in the illustration. Hold for 30 seconds. Relax and repeat.
- Forward flexion — supine position. Lie on your back with your legs straight. Use your unaffected arm to lift your affected arm overhead until you feel a gentle stretch. Hold for 15 seconds and slowly lower to start position. Relax and repeat.
- Crossover arm stretch. Gently pull one arm across your chest just below your chin as far as possible without causing pain. Hold for 30 seconds. Relax and repeat.
Tips and Tricks for successful non-operative treatment
• Ensure you keep your shoulder as mobile as you are able, using your arm as much as you can to help with your daily activities
• Adequately control your pain, pain stops you being able to move the arm and may result in the shoulder becoming more restricted. Speak to a pharmacist if you are unsure which medication may help
• You could apply heat or ice to help with the pain and healing. Ensure that you do not apply these directly to the skin. Also do not use them too frequently or for prolonged periods of time (up to 20 minutes), as these treatments can burn the skin• Try to maintain a good posture
Surgical options
If your symptoms are not relieved by therapy and other conservative methods, you and your doctor may discuss surgery. It is important to talk with your doctor about your potential for recovery continuing with simple treatments, and the risks involved with surgery.
Surgery for frozen shoulder is typically offered during “Stage 2: Frozen.” The goal of surgery is to stretch and release the stiffened joint capsule. The most common methods include manipulation under anesthesia and shoulder arthroscopy.
Manipulation under anesthesia. During this procedure, you are put to sleep. Your doctor will force your shoulder to move which causes the capsule and scar tissue to stretch or tear. This releases the tightening and increases range of motion. This might carry the risk of fracture.
Shoulder arthroscopy. In this procedure, your doctor will cut through tight portions of the joint capsule. This is done using pencil-sized instruments inserted through small incisions around your shoulder.
In many cases, manipulation and arthroscopy are used in combination to obtain maximum results. Most patients have good outcomes with these procedures.
Am I damaging my shoulder?
You will not damage your shoulder by performing routine daily chores and tasks as best as you can tolerate, the pain with a frozen shoulder does not usually indicate any harm.
We recommend undertaking our shoulder reconditioning program.
Do I need any investigations?
There is no specific test to help diagnose a frozen shoulder, but occasionally your GP or physiotherapist may request further investigations, such as an X-ray. An MRI scan is recommended to exclude other structural abnormalities.
Adhesive capsulitis Flow Chart