1. Introduction to Arm Tendonitis
Arm tendonitis, also known as tendinitis, is a condition characterized by inflammation or irritation of the tendons in the arm. Tendons are the fibrous connective tissues that attach muscles to bones, facilitating movement and force transmission. When these tendons are overused, injured, or subjected to repetitive stress, microscopic damage can occur, leading to inflammation and pain.
Tendonitis can affect any part of the arm, including the shoulder, elbow, wrist, or forearm. The most common forms include:
- Lateral epicondylitis (Tennis Elbow)
- Medial epicondylitis (Golfer’s Elbow)
- Rotator Cuff Tendonitis
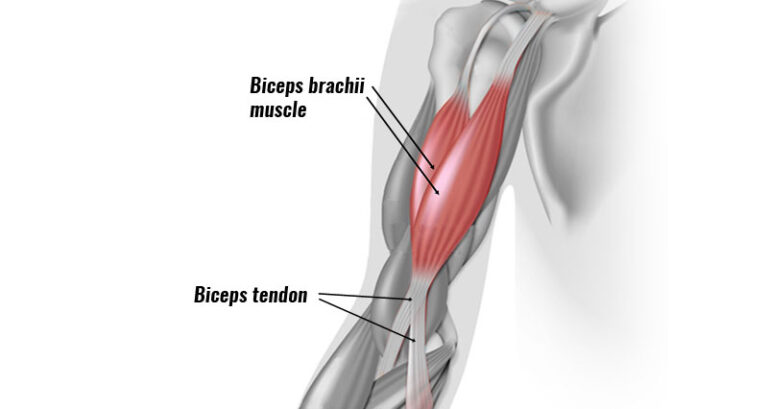
- Biceps Tendonitis
- Wrist Flexor or Extensor Tendonitis
Arm tendonitis is a prevalent musculoskeletal condition, particularly among athletes, manual laborers, and individuals who engage in repetitive arm movements. While it is not life-threatening, untreated tendonitis can severely impair arm function and quality of life.
This article presents an evidence-based review of the most effective treatments for arm tendonitis, ranging from conservative management to advanced therapies and surgical interventions.
2. Causes and Risk Factors
Arm tendonitis develops when tendons undergo repeated strain or acute trauma. Several risk factors contribute to the development of this condition:
2.1 Repetitive Motion and Overuse
Occupational or athletic activities that involve repetitive arm movements—such as typing, painting, lifting weights, playing tennis, or carpentry—can cause cumulative tendon stress, leading to inflammation and degeneration.
2.2 Poor Technique or Posture
Incorrect posture during work or improper techniques in sports can place excessive stress on tendons. This mechanical overload increases the risk of microtears and inflammation.
2.3 Age-Related Degeneration
As individuals age, tendons naturally lose elasticity and hydration, becoming more prone to injury. Tendon degeneration, or tendinosis, may also occur alongside inflammation.
2.4 Systemic Conditions
Certain health conditions, such as rheumatoid arthritis, diabetes, or thyroid disorders, may impair tendon healing and increase susceptibility to tendonitis.
2.5 Trauma or Sudden Force
A single, forceful impact or overexertion of the arm may cause acute tendon inflammation or partial tendon tears.
3. Clinical Presentation and Diagnosis
3.1 Symptoms
The typical symptoms of arm tendonitis include:
- Pain localized to the tendon region
- Swelling and tenderness over the affected area
- Stiffness and reduced range of motion
- Pain worsening with activity or specific movements
- A sensation of heat or redness in inflamed areas
3.2 Diagnostic Methods
Diagnosis is primarily clinical, based on history and physical examination. Diagnostic imaging may be used to confirm the diagnosis or rule out other conditions.
3.2.1 Physical Examination
- Palpation of tendons for tenderness
- Resistance tests to identify the affected tendon
- Range of motion and strength assessments
3.2.2 Imaging Techniques
- Ultrasound: Useful for detecting fluid accumulation and structural damage in soft tissues.
- MRI: Provides high-resolution images of tendon fibers and associated joint structures.
- X-rays: Help identify calcific tendonitis or bone abnormalities but have limited utility for soft tissue visualization.
4. Conservative Treatment Options
Conservative management is typically the first-line approach for arm tendonitis and has proven effective in most cases. These treatments aim to reduce inflammation, relieve pain, and promote tendon healing without surgical intervention.
4.1 Rest and Activity Modification
Rest is fundamental to allowing the inflamed tendon to recover. Patients are advised to:
- Avoid or minimize activities that aggravate symptoms
- Take frequent breaks during repetitive tasks
- Use ergonomic modifications at workstations Activity modification, rather than complete immobilization, is often preferred to prevent muscle atrophy and joint stiffness.
4.2 Ice Therapy and Compression
Applying ice packs to the affected area helps reduce inflammation and pain. Best practices include:
- Applying ice for 15–20 minutes, 3–4 times daily
- Avoiding direct skin contact to prevent frostbite Compression wraps or sleeves can minimize swelling and provide mild support.
4.3 Physical Therapy and Stretching
A customized physical therapy program is a cornerstone of conservative treatment. It may include:
- Stretching exercises: To improve flexibility and reduce tendon strain
- Eccentric strengthening: Exercises that lengthen the tendon under tension, which has shown superior efficacy in treating chronic tendonitis
- Range-of-motion exercises: To maintain joint mobility
- Manual therapy: Techniques such as soft tissue mobilization or trigger point release
4.4 Non-Steroidal Anti-Inflammatory Drugs (NSAIDs)
NSAIDs like ibuprofen or naproxen are commonly used to control pain and reduce inflammation. They are typically prescribed for short-term use due to potential side effects such as gastrointestinal irritation or renal complications.
4.5 Orthotics and Bracing
Supportive devices can relieve tendon strain during daily activities:
- Elbow braces (e.g., counterforce bands) for lateral or medial epicondylitis
- Wrist splints for wrist tendonitis
- Shoulder slings or posture correctors for rotator cuff tendonitis These aids reduce tendon tension, particularly during repetitive arm motions.
5. Advanced Non-Surgical Treatments
When conservative measures fail to provide adequate relief, several advanced therapies may be recommended. These options are backed by growing clinical evidence and are often used in chronic or refractory tendonitis cases.
5.1 Corticosteroid Injections
Corticosteroids are potent anti-inflammatory agents that offer short-term pain relief when injected around the tendon sheath. However, repeated injections are discouraged due to potential side effects such as:
- Tendon weakening or rupture
- Skin thinning and depigmentation
- Localized infection risk
5.2 Platelet-Rich Plasma (PRP) Therapy
PRP therapy involves injecting the patient’s own concentrated platelets into the tendon area. Platelets release growth factors that stimulate healing and tissue regeneration. Clinical studies suggest:
- Improved outcomes in chronic tendonitis compared to corticosteroids
- Fewer adverse effects
- Best results when combined with physical therapy
5.3 Shockwave Therapy (Extracorporeal Shockwave Therapy – ESWT)
ESWT uses acoustic waves to promote tissue healing and neovascularization. This non-invasive treatment:
- Is effective for chronic calcific tendonitis and epicondylitis
- May require multiple sessions
- Has minimal side effects such as temporary soreness
5.4 Ultrasound-Guided Dry Needling
This technique uses fine needles to puncture the tendon and promote a local healing response. It may be combined with autologous blood or PRP injections. It is typically performed under ultrasound guidance to ensure precision.
5.5 Laser Therapy (Low-Level Laser Therapy – LLLT)
LLLT uses low-intensity lasers to stimulate cellular repair processes. Though evidence is mixed, some studies report:
- Reduction in pain and inflammation
- Improved tissue healing
- Faster return to activity when used adjunctively
6. Surgical Interventions
Surgical treatment is reserved for patients who do not respond to conservative and advanced non-surgical treatments after 6–12 months.
6.1 Tendon Debridement
This procedure involves removing degenerated tendon tissue and any calcific deposits. It helps reduce pain and stimulate the healing of healthy tendon fibers.
6.2 Tendon Repair or Reattachment
In cases of partial or complete tendon tears, surgical repair is performed to restore tendon continuity. Techniques include:
- Suturing the tendon back to the bone
- Tendon grafting in complex cases
6.3 Minimally Invasive Arthroscopic Techniques
Arthroscopy offers a less invasive approach with faster recovery and minimal scarring. Procedures include:
- Tendon debridement
- Subacromial decompression for rotator cuff tendonitis
- Synovectomy in chronic inflammatory cases
6.4 Postoperative Care
Post-surgical recovery involves immobilization followed by a structured rehabilitation program. Full recovery may take several months depending on the extent of surgery.
7. Rehabilitation and Recovery
Rehabilitation is an essential phase in the recovery process from arm tendonitis, whether the condition is managed conservatively or surgically. A structured rehabilitation plan ensures tissue healing, restores functional movement, and prevents recurrence.
7.1 Post-Treatment Physiotherapy
After acute symptoms subside, a carefully designed physiotherapy program is crucial to restore mobility, strength, and endurance in the affected arm. Key components include:
- Progressive stretching exercises: Improve tendon flexibility and joint range of motion.
- Resistance and strengthening exercises: Target the affected muscle groups and tendons to enhance load tolerance.
- Proprioceptive training: Improves neuromuscular control and joint stabilization.
- Therapeutic modalities: Ultrasound therapy, electrical stimulation, and cold laser therapy may aid tissue repair.
7.2 Occupational Therapy
In cases where tendonitis affects daily work functions, occupational therapy can assist patients in adapting activities and work environments. Therapists may:
- Suggest ergonomic improvements
- Teach joint protection techniques
- Recommend adaptive tools or braces
7.3 Return-to-Activity Protocols
Gradual return-to-activity is essential to avoid reinjury:
- Phase I: Symptom control and gentle movement
- Phase II: Restoration of strength and flexibility
- Phase III: Functional training and endurance exercises
- Phase IV: Return to sports or work with progressive load
Protocols vary based on tendon location, treatment type, and individual progress.
8. Preventive Strategies
Prevention of arm tendonitis is as important as treatment. Implementing proactive strategies can significantly reduce the risk of recurrence or chronic progression.
8.1 Ergonomic Adjustments
Proper ergonomics in work and sports can reduce tendon strain:
- Use adjustable chairs and desks
- Maintain wrist neutrality while typing
- Optimize tool grip and arm positioning
- Avoid prolonged static postures
8.2 Proper Warm-Up and Stretching
A warm-up routine increases blood flow and muscle temperature, reducing tendon injury risk:
- Dynamic stretching before activity
- Static stretching post-exercise to maintain flexibility
8.3 Strengthening Exercises
Regular strength training builds muscle support around tendons, reducing mechanical load. Focus areas:
- Forearm muscles (flexors and extensors)
- Shoulder stabilizers (rotator cuff, scapular muscles)
- Elbow and wrist stabilizers
8.4 Technique Refinement
In sports and repetitive tasks, learning proper techniques from coaches or therapists can prevent abnormal tendon loading. Small adjustments in posture, grip, and movement patterns can make a significant difference.
9. Complications and Long-Term Outcomes
Although most tendonitis cases resolve with treatment, complications can occur if not managed properly.
9.1 Chronic Tendonitis and Tendinosis
Persistent inflammation can evolve into tendinosis, marked by tendon degeneration rather than inflammation. This condition:
- Responds poorly to NSAIDs or corticosteroids
- Requires regenerative therapies or surgery
9.2 Tendon Rupture
Repeated corticosteroid injections or neglected severe tendonitis can weaken tendons, increasing the risk of complete rupture—a condition requiring surgical repair.
9.3 Adhesions and Joint Stiffness
Immobilization or inadequate rehabilitation may cause adhesions or joint contractures, reducing range of motion.
9.4 Recurrence
Return to activity without adequate recovery or addressing underlying risk factors can lead to relapse.
9.5 Prognosis
With early diagnosis and appropriate treatment:
- Most patients recover fully within 6–12 weeks
- Chronic cases may take several months
- Surgical outcomes are generally favorable but depend on tendon condition and rehabilitation
10. Case Studies and Clinical Trial Evidence
Clinical evidence supports various treatment strategies for arm tendonitis:
10.1 PRP vs Corticosteroid Injections
A meta-analysis published in The American Journal of Sports Medicine showed PRP therapy offers superior long-term pain relief and functional improvement compared to corticosteroids in lateral epicondylitis.
10.2 Eccentric Training
Studies have consistently shown that eccentric strengthening exercises are more effective than traditional concentric training for chronic tendonitis.
10.3 Shockwave Therapy Trials
Randomized controlled trials have confirmed that ESWT significantly improves pain and function scores in patients with chronic calcific tendonitis and lateral epicondylitis.
10.4 Surgical Outcomes
Long-term studies indicate that tendon debridement and arthroscopic repair have high success rates, especially when followed by a structured rehabilitation plan.
11. Frequently Asked Questions (SEO Section)
• What is the fastest way to recover from arm tendonitis?
Rest, ice, anti-inflammatory medications, and early physical therapy are the most effective initial steps. PRP therapy and shockwave therapy may speed up recovery in chronic cases.
• How long does it take for arm tendonitis to heal?
Mild to moderate cases usually heal in 6–12 weeks. Chronic or severe cases may require several months, especially if surgery is needed.
• Is massage good for tendonitis in the arm?
Yes, therapeutic massage can help improve circulation, reduce stiffness, and promote tendon healing when performed by trained professionals.
• Can I exercise with arm tendonitis?
Light stretching and guided physical therapy exercises are beneficial. However, high-impact or aggravating movements should be avoided until recovery progresses.
• Do tendonitis braces really work?
Braces reduce strain on the affected tendon during activity and can provide symptomatic relief, especially in epicondylitis and wrist tendonitis.