Definition
Distal radioulnar joint (DRUJ) instability can be acute or chronic, unidirectional (volar or dorsal) or bidirectional, and isolated or associated with other injuries. Clinically significant instability is often identified by increased anteroposterior translation of the DRUJ with passive manipulation compared to the normal side. DRUJ dislocation or instability is described based on the position of the ulnar head relative to the distal radius.
Anatomy
The DRUJ comprises the articulation between the ulnar head and the sigmoid notch of the distal radius, along with supporting soft tissues. The DRUJ is not congruent, with the sigmoid notch’s curvature typically 50% greater than the ulnar head’s. The soft tissue structures contributing to DRUJ stability include the pronator quadratus, extensor carpi ulnaris (ECU) and its sheath, interosseous membrane, DRUJ capsule, and components of the triangular fibrocartilage complex (TFCC). Multiple structures must be injured to result in joint instability. The prime stabilizers of the DRUJ within the TFCC are the palmar and dorsal radioulnar ligaments.
Pathogenesis
DRUJ injury commonly results from a distal radius fracture. Angulation greater than 20 to 30 degrees distorts the TFCC and alters joint kinematics. Radius shortening by more than 5 to 7 mm can rupture the distal radioulnar ligaments. Fractures at the ulnar styloid base can also disrupt the radioulnar ligaments, causing instability. Isolated dorsal DRUJ dislocations are typically caused by forceful hyperpronation and wrist extension, while volar dislocations occur from supinated forearm injuries, forceful torque, or direct blows to the forearm.
Natural History
Delayed diagnosis and treatment of acute DRUJ injuries lead to worse outcomes, and chronic instability rarely improves spontaneously. There is no proven link between DRUJ instability and symptomatic arthritis development, although some degeneration is expected with recurrent dislocations.
Patient History and Physical Findings
Patients often report falling on an outstretched hand or experiencing forced wrist rotation, followed by ulnar-sided wrist pain and swelling. Chronic instability may present as a clunk during forearm rotation, and pain and weakness are exacerbated by activities requiring forceful rotation while gripping. Increased passive volar-dorsal translation of the ulna relative to the radius indicates DRUJ instability.
For acute distal radius fractures with DRUJ disruption, the fracture should be reduced and stabilized first, then the DRUJ should be assessed compared to the uninjured wrist. Typically, distal radius fracture management alone adequately treats the DRUJ. Patients with DRUJ instability usually maintain full or nearly full wrist range of motion. A thorough examination should include:
- Passive translation (“piano key” sign): Compare results to the unaffected side in various positions.
- Modified press test: Increased depression of the ulnar head on the affected side indicates instability.
- Passive forearm rotation: A painful clunk indicates joint dislocation and gross DRUJ instability.
Imaging and Other Diagnostic Studies
- Posteroanterior (PA) view: Obtain with the humerus abducted, elbow flexed, and forearm on a flat surface to check for:
- Displaced fractures at the ulnar styloid base
- Fleck fractures from the fovea of the ulnar head
- Widening of the DRUJ
- Acquired positive ulnar variance greater than 5 mm compared to the opposite wrist
- Lateral radiograph: Obtain with the arm at the patient’s side and elbow flexed 90 degrees for accurate DRUJ alignment assessment.
- Computed tomography (CT): Perform on both wrists, with axial images in identical rotations, preferably in neutral and maximum pronation and supination.
- Magnetic resonance imaging (MRI): Detects TFCC tears, though its sensitivity and specificity depend on the technique. It can also assess the shape of the sigmoid notch and joint stability.
Differential Diagnosis
- ECU tendonitis or subluxation
- Ulnar impaction syndrome
- DRUJ arthritis
- Pisotriquetral arthritis
- Lunotriquetral ligament tear
- TFCC disc tear
Nonoperative Management
Mild chronic instability may be managed with nonsteroidal anti-inflammatory drugs (NSAIDs), a splint limiting forearm rotation, and a forearm strengthening program. Prolonged conservative management is recommended for patients with generalized ligamentous laxity and bilateral DRUJ instability before considering surgery.
Surgical Management
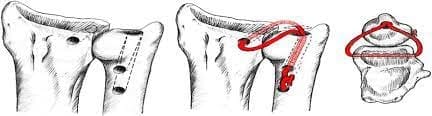
Distal radioulnar ligament reconstruction is indicated for chronic DRUJ instability where the TFCC is inadequate for primary repair due to chronicity or severity. The goal is to restore DRUJ stability and provide a full, painless range of forearm motion through near-anatomic reconstruction of the dorsal and volar radioulnar ligaments. Osseous malalignment or sigmoid notch deficiency must be addressed during ligament reconstruction for a durable result.
Preoperative Planning
Review imaging studies for evidence of osseous deformity or DRUJ articular surface degeneration. A competent sigmoid notch is required for successful intra-articular radioulnar ligament reconstruction. Plan the tendon graft source, typically the palmaris longus (PL) tendon, or alternatives like the plantaris, extensor digitorum longus, or a flexor carpi ulnaris tendon strip.