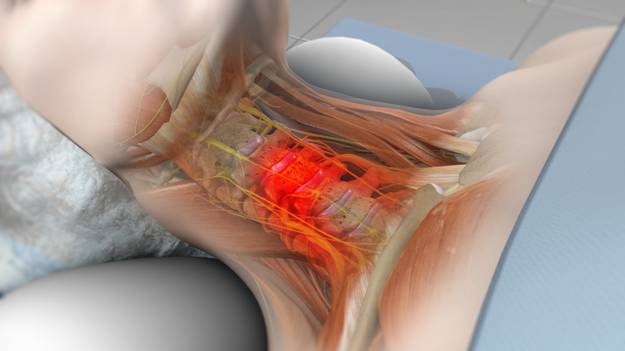
This article discusses surgical options for cervical radiculopathy. For general information, see Cervical Radiculopathy (Pinched Nerve).
If symptoms of cervical radiculopathy persist or worsen despite nonsurgical treatments, surgery may be recommended by your doctor.
The primary goal of surgery is to alleviate symptoms by decompressing, or relieving pressure on, the compressed nerves in the neck. Additional goals include:
- Improving neck pain
- Maintaining spinal stability
- Correcting spinal alignment
- Preserving neck range of motion
Typically, surgery involves removing parts of bone, soft tissue (such as a herniated disk), or both to create more space for the nerves to exit the spinal canal.
Surgical Procedures
Three common surgical procedures for treating cervical radiculopathy are:
- Anterior cervical diskectomy and fusion (ACDF)
- Artificial disk replacement, or arthroplasty (ADR)
- Posterior cervical laminoforaminotomy
The choice of procedure depends on several factors, including the type and location of the problem, patient preferences, the surgeon’s experience, and the patient’s overall health and medical history, including prior neck surgeries.
Anterior Cervical Diskectomy and Fusion (ACDF)
ACDF is the most common procedure for cervical radiculopathy. It involves removing the problematic disk or bone spurs and stabilizing the spine through fusion.
The goals of ACDF are to:
- Restore spinal alignment
- Maintain space for nerve roots to exit the spine
- Limit motion across the degenerated spinal segment
Procedure:
An “anterior” approach means the doctor will operate through a 1- to 4-inch incision in the front of the neck. The exact location and length of the incision depend on the specific condition.
During the procedure:
- The problematic disk and any additional bone spurs are removed.
- A bone graft or spacer is placed in the space where the disk was, restoring disk space height and allowing more room for nerves to exit the spine.
- Spinal fusion stabilizes the spine by “welding” vertebrae together to heal into a single, solid bone, eliminating motion between degenerated vertebrae and reducing pain.
Most spinal fusions use bone grafts, which may come from:
- The patient’s own bone (autograft), typically taken from the hip, requiring an additional incision and potentially causing post-operative pain.
- A donor (allograft).
In some cases, a metal cage containing bone graft material is implanted between vertebrae. Metal screws and plates may be used to enhance fusion and stabilize the spine.
Artificial Disk Replacement (ADR)
This procedure involves removing the degenerated disk and replacing it with an artificial disk to maintain flexibility and normal motion.
Like ACDF, ADR uses an “anterior” approach with an incision along the neck crease. The problematic disk is removed, and an artificial disk implant is inserted. The implant:
- May be made of all metal or a combination of metal and plastic.
- Is designed to maintain motion between vertebrae and restore the height between vertebrae, widening the nerve passageway.
Although ADR is newer than spinal fusion, short-term outcomes are promising and comparable to fusion surgery. Long-term outcomes are still under study. ADR may be an option based on the type and location of the problem, and should be discussed with your doctor.
Posterior Cervical Laminoforaminotomy
“Posterior” refers to the back part of the body. During this procedure, a 1- to 2-inch incision is made along the midline of the back of the neck. The exact location and size depend on the condition.
The doctor thins the lamina (bony arch) to access the damaged nerve and removes bone, bone spurs, and tissues compressing the nerve. If a herniated disk is involved, the compressing portion is also removed.
Unlike ACDF, this procedure does not always require spinal fusion, allowing for maintained neck motion and quicker recovery. It can be performed as open surgery or using minimally invasive methods.
Complications
As with any surgery, risks are involved. Potential complications can be related to the surgical approach, bone grafts, healing, and long-term changes. General risks include:
- Infection
- Bleeding
- Nerve injury
- Spinal cord injury
- Anesthesia reactions
- Need for additional surgery
- Failure to relieve symptoms
- Dural tear (tear of the sac covering the nerves)
- Life-threatening complications (heart attack, lung issues, stroke)
Additional risks for anterior approaches include:
- Misplaced, broken, or loosened implants
- Swallowing difficulties
- Voice changes
- Breathing difficulties
- Esophagus injury
- Pain at the bone graft site
- Nonunion of the spinal fusion (in ACDF)
Recovery
Post-surgery, patients typically stay in the hospital for one night, though some may go home the same day. Recovery time varies based on the surgery type, the number of disk levels involved, and overall health.
Most patients can walk and eat the day after surgery, though swallowing solid foods may be difficult for a few weeks, and some hoarseness may occur following anterior cervical spine surgery.
Patients may need to wear a cervical collar initially, with the duration depending on the surgery type. Spinal fusion recovery may take 6 to 12 months for solid bone formation, during which specific activity restrictions are advised. Light activities, such as walking, are recommended immediately after surgery, with gradual increases in activity as strength returns.
Physical Therapy
By 4 to 6 weeks post-surgery, patients can begin range-of-motion and strengthening exercises. Physical therapy may be prescribed to aid in regaining full function.
Return to Work
Most patients can return to desk jobs within a few days to weeks after surgery and to full activities by 3 to 4 months, depending on the procedure. Healing times may vary for some individuals.
Outcomes
Most patients experience favorable outcomes, with significant pain relief and a return to daily activities after recovery.