Introduction
Cervical foraminotomy is a surgical procedure designed to enlarge the neural foramen, the bony opening through which spinal nerve roots exit the cervical spine. The term “foramen” refers to the opening surrounding the nerve root, while “otomy” signifies the surgical technique used to widen this space. The goal of the procedure is to **alleviate nerve compressioalleviate nerve compression, reducing pain, numbness, and weakness caused by conditions such as **herniated discs, boherniated discs, bone spurs, or degenerative changes.
This guide provides insight into:
The indicatioThe indications for cervical foraminotomy
The surgical objectives anThe surgical objectives and expected outcomes
Postoperative recovery and rehabilitation
Anatomy of the Cervical Spine
What Structures Are Affected?
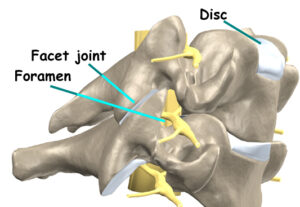
The cervical spine consists of seven vertebrae (C1-C7), forming the uppermost segment of the spinal column. Each vertebra is composed of a vertebral body at the front and a bony arch at the back, enclosing the spinal canal—a protective passageway housing the spinal cord.
Between adjacent vertebrae are intervertebral discs, which act as shock absorbers and contribute to spinal flexibility.
The Neural Foramina and Nerve Compression
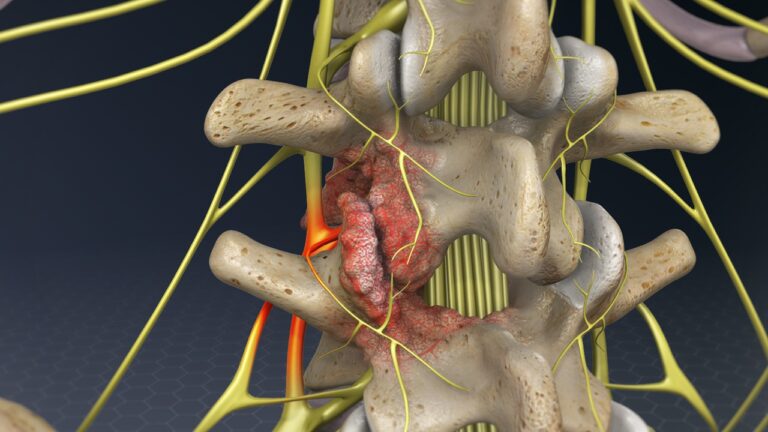
As the spinal cord extends downward from the brain, it gives rise to nerve roots that pass through paired neural foramina on either side of each vertebra. These foramina serve as crucial exit points for nerves that control sensation and movement in the upper limbs.
However, certain spinal conditions can narrow the foramina, leading to nerve compression (foraminal stenosis). Common causes include:
- Herniated or Bulging Discs – The intervertebral disc sits just in front of the foramen. When a disc bulges or herniates, it can encroach upon the space, exerting pressure on the nerve root.
- Facet Joint Hypertrophy & Bone Spurs – The facet joints, located behind the foramen, may develop bone spurs (osteophytes) due to degenerative arthritis. These bony projections further narrow the passage, causing nerve irritation and pain.
- Degenerative Disc Disease – Over time, intervertebral discs lose hydration and collapse, leading to a reduction in foraminal height and increased pressure on exiting nerve roots.
By widening the foraminal space, cervical foraminotomy aims to relieve nerve compression, restore function, and improve quality of life for individuals experiencing cervical radiculopathy (nerve pain radiating to the arms and shoulders).
Rationale for Cervical Foraminotomy
What is the Goal of Surgery?
Cervical foraminotomy is performed to relieve symptoms of foraminal stenosis, a condition where a nerve root is compressed within the neural foramen. This compression typically results from degenerative changes in the cervical spine, which develop over time due to repetitive stress and strain on the neck.
• Degenerative changes can lead to the gradual collapse of intervertebral discs, reducing the space between vertebrae and narrowing the foraminal opening, which increases pressure on the nerve root.
• As degeneration progresses, the facet joints lining the foramen become inflamed and enlarge, further contributing to nerve compression.
• Bone spurs (osteophytes) may form along the edges of the foramen, exacerbating nerve irritation and worsening symptoms.
During a foraminotomy, the surgeon removes excess bone and soft tissue around the foramen, effectively widening the opening and alleviating pressure on the compressed nerve root. This helps reduce pain, numbness, and weakness associated with nerve compression.
Preoperative Preparations
How Should I Prepare for Surgery?
The decision to proceed with cervical foraminotomy should be made in collaboration with your surgeon, ensuring that you fully understand the procedure, potential risks, and expected outcomes. If you have any questions or concerns, discuss them with your healthcare provider before finalizing your decision.
Once surgery is scheduled, several preoperative steps may be necessary:
• Your surgeon may recommend a comprehensive physical examination by your primary care physician to ensure you are in optimal health for the procedure.
• If you take medications, particularly blood thinners or anti-inflammatory drugs, your doctor will provide instructions on whether any adjustments are necessary before surgery.
• On the day of surgery, you will likely be admitted to the hospital early in the morning.
• To reduce the risk of complications, avoid eating or drinking after midnight the night before your procedure.
Surgical Procedure
What Happens During the Operation?
Cervical foraminotomy is typically performed under general anesthesia, ensuring the patient is asleep and pain-free during the procedure.
• For shorter spinal surgeries such as foraminotomy, anesthesia is usually administered as a gas through a mask.
• During the procedure, a ventilator may be used to assist breathing and regulate airflow to the lungs.
Patient Positioning and Incision
• The patient is positioned face down on the operating table to allow optimal access to the cervical spine.
• The surgeon makes a small incision along the midline of the back of the neck.
• Soft tissues are carefully retracted to expose the affected neural foramen where the spinal nerve is compressed.
Surgical Technique
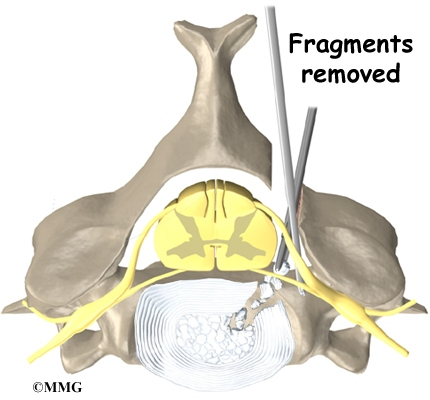
• Some surgeons use a surgical microscope to magnify the area, enhancing precision during the procedure.
• A small rotary cutting tool (burr) may be used to shave the inside edge of the facet joint, expanding the foraminal opening.
• In some cases, a portion of the bony ring (lamina) from the vertebrae above and below the affected nerve may be removed to improve decompression.
• Small surgical instruments are used to carefully extract soft tissues, remove herniated disc fragments, and scrape off bone spurs that contribute to nerve compression.
By widening the foramen and removing obstructions, the surgeon relieves tension and pressure on the nerve root, improving mobility and reducing pain.
The muscles and soft tissues are put back in place, and the skin is stitched together. Patients are sometimes placed in a soft collar after surgery to keep the neck positioned comfortably.
Complications of Cervical Foraminotomy
What Are the Potential Risks?
As with any major surgical procedure, complications may arise following a cervical foraminotomy. While the risk is generally low, it is essential to understand potential postoperative concerns. Some of the most common complications include:
• Problems with anesthesia
• Thrombophlebitis (blood clots)
• Infection
• Nerve damage
• Persistent or recurrent pain
This list is not exhaustive, but these represent the most frequently encountered complications.
Problems with Anesthesia
Complications related to anesthesia may occur when a patient’s existing medications interact with the anesthetic agents. Though rare, some individuals may have an adverse reaction to the anesthesia itself. Additionally, general anesthesia can temporarily impact lung function, as breathing is assisted by a ventilator during the procedure. Patients with preexisting lung conditions should discuss potential risks with their anesthesiologist before surgery.
Thrombophlebitis (Blood Clots / Deep Vein Thrombosis – DVT)
Thrombophlebitis, commonly referred to as deep vein thrombosis (DVT), can occur after any surgical procedure. It results from the formation of blood clots in the deep veins of the legs, potentially leading to swelling, warmth, and pain. If a clot dislodges and travels to the lungs, it may cause a pulmonary embolism, a severe and potentially life-threatening condition.
To minimize the risk of DVT, surgeons implement preventative measures, including:
• Early mobilization – Encouraging patients to move as soon as possible after surgery
• Compression stockings – Special stockings that help maintain circulation in the legs
• Anticoagulant medications – Blood thinners that reduce the likelihood of clot formation
Infection
Postoperative infection is uncommon following spine surgery but can be a serious complication if it occurs. Superficial wound infections generally respond well to oral antibiotics, whereas deep infections affecting the spinal structures may require intravenous antibiotics or additional surgery. Some infections develop before hospital discharge, while others may appear weeks after surgery.
Signs of infection include:
• Redness, swelling, or increased pain at the incision site
• Drainage of pus or an unusual odor
• Fever or chills
Nerve Damage
Given that cervical foraminotomy is performed near spinal nerves, there is a small risk of nerve injury. This may result from direct trauma during surgery, postoperative swelling, or the formation of scar tissue around the nerve root. Damage to spinal nerves can lead to:
• Muscle weakness
• Sensory disturbances (numbness or tingling in the arms or hands)
• Persistent pain
Most nerve-related symptoms resolve over time, but in rare cases, some neurological deficits may persist.
Persistent or Recurrent Pain
While most patients experience significant pain relief, some individuals may have ongoing or recurrent symptoms. This may result from:
• Incomplete decompression of the nerve root
• Postoperative scar tissue formation
• Underlying degenerative spine disease
If pain persists, further evaluation through imaging studies and additional treatments may be required.
Postoperative Care: What to Expect After Surgery
Following cervical foraminotomy, patients are encouraged to mobilize within a few hours after surgery. Depending on the surgeon’s preference, some individuals may be advised to wear a soft cervical collar for additional support.
• Most patients are discharged within 24 hours
• Driving is typically safe within 1-2 weeks
• Light work can often resume by four weeks
• Full return to strenuous activities and sports generally occurs within two to three months
For patients experiencing significant muscle weakness or prolonged discomfort, outpatient physical therapy may be recommended.
Rehabilitation and Recovery
What to Expect During Rehabilitation?
Rehabilitation following cervical foraminotomy is usually short-term and focuses on gradual recovery of strength and mobility. Patients requiring physical therapy typically attend sessions for two to four weeks, with full recovery expected within two to three months.
Early Postoperative Rehabilitation
Many surgeons initiate physical therapy within four weeks post-surgery. Initially, treatments are aimed at reducing pain and inflammation through:
• Ice therapy and electrical stimulation – Helps control swelling and discomfort
• Massage therapy and manual techniques – Relieves muscle spasms and promotes circulation
Progressive Rehabilitation and Strengthening
As recovery progresses, active rehabilitation begins, incorporating:
• Cardiovascular exercises – Walking, stationary cycling, and arm cycling to improve endurance
• Neck and upper back stabilization exercises – Designed to strengthen supporting muscles
• Postural training and movement correction – Helps patients relearn safe and efficient movement patterns
Body mechanics training is an essential part of rehabilitation, focusing on how to safely perform daily activities such as:
• Getting in and out of bed
• Lifting and carrying objects
• Returning to work-related tasks
For patients whose jobs involve heavy lifting or physically strenuous activities, therapists may modify work tasks or suggest alternative roles to prevent further strain on the cervical spine.
Preventing Future Issues
Before discharge from therapy, patients are educated on strategies to minimize the risk of recurrence. This includes:
• Maintaining proper posture to avoid excessive neck strain
• Using ergonomic adjustments at work to reduce repetitive stress on the cervical spine
• Performing regular stretching and strengthening exercises to promote spinal health
By following these recommendations, patients can enhance their long-term recovery and reduce the likelihood of future cervical spine issues.