Introduction
Understanding Cervical Corpectomy and Strut Graft Surgery
A cervical corpectomy is a surgical procedure designed to relieve spinal cord compression caused by spinal stenosis. Spinal stenosis occurs when bone spurs exert pressure on the spinal cord, leading to a condition known as myelopathy. Symptoms of myelopathy may include:
- Bowel and bladder dysfunction
- Gait disturbances (difficulty walking)
- Impaired fine motor skills, particularly in the hands
During a corpectomy, the front portion of the spinal column (vertebral body) is removed to alleviate this pressure. The term “corpectomy” comes from “corpus” meaning body and “ectomy” meaning removal. To stabilize the spine and maintain its structure, the removed area is filled with bone grafts or synthetic materials.
This procedure is typically performed when bone spurs affect multiple vertebrae, making less invasive treatments ineffective.
This guide explains:
- The affected parts of the spinal column
- Why cervical corpectomy becomes necessary
- What to expect before and during the surgery
- Recovery and rehabilitation after the operation
Anatomy
What Parts of the Neck Are Involved in a Cervical Corpectomy?
The cervical corpectomy procedure is performed through the anterior neck region, or the front of the neck. This approach allows surgeons to access and treat key structures, including:
- Ligaments: Connective tissues that support the spine and maintain stability.
- Bones: Specifically, the vertebral bodies that form the spinal column.
- Intervertebral Discs: Cushions between the vertebrae that absorb shock and facilitate movement.
- Spinal Cord and Nerves: Critical components responsible for transmitting signals between the brain and body.
This approach provides a clear path to address spinal compression effectively while minimizing disruption to surrounding structures.
Rationale
What Are the Goals of Cervical Corpectomy Surgery?
Spinal stenosis develops when bone spurs intrude into the spinal canal, compressing the spinal cord. This compression can lead to symptoms such as pain, numbness, weakness, or impaired motor function.
The primary goal of a cervical corpectomy is to:
- Alleviate Spinal Cord Compression: By removing the affected vertebral bodies along the front section of the spinal column, surgeons can relieve pressure on the spinal cord’s anterior surface.
- Reduce or Eliminate Symptoms: This includes addressing issues like myelopathy, improving nerve function, and restoring mobility and quality of life.
By clearing the obstructive bone spurs, the procedure provides the spinal cord with the space needed to function without irritation or compression.
Preparations
How Should You Prepare for a Cervical Corpectomy?
The decision to undergo a cervical corpectomy is made collaboratively between you and your surgeon. It is essential to fully understand the procedure and address any questions or concerns with your doctor before proceeding.
Preoperative Steps
- Physical Examination:
Your surgeon may recommend a thorough evaluation by your primary care physician to ensure you are in optimal health for surgery. This step helps identify and address any conditions that could affect the procedure or recovery. - Fasting Before Surgery:
You should avoid eating or drinking anything after midnight the night before the operation. This reduces the risk of complications during anesthesia. - Admission on Surgery Day:
You will likely be admitted to the hospital early in the morning on the day of your surgery. Be prepared to follow all preoperative instructions provided by your surgical team.
By following these preparation guidelines, you can ensure the surgery proceeds smoothly and safely.
Surgical Procedure
What Happens During a Cervical Corpectomy?
A cervical corpectomy is a detailed procedure performed under general anesthesia, ensuring the patient is asleep and comfortable. Here is a step-by-step breakdown of the surgery:
1. Preparation and Initial Incision
- An incision is made along the left side of the neck, extending toward the ear and under the jaw to the chin.
- The skin flap is lifted to expose the neck structures, and retractors are used to gently separate muscles and soft tissues, providing access to the spine.
2. Mild Traction
- Special instruments are attached to either the skull or spinal bones to apply gentle traction, stretching the neck slightly.
- This creates more room for the surgeon to work and reduces pressure on the spinal cord.
3. Locating and Removing Vertebral Structures
- A needle is inserted into the disc space, and an X-ray is used to identify the target sections of the spine.
- The anterior longitudinal ligament (a strong tissue running along the spine) is partially removed.
- Discectomy: The front and back portions of the discs between the vertebrae are carefully removed.
- Corpectomy: A rotary tool (burr) is used to excise the vertebral bodies while leaving the protective ring of bone around the spinal cord intact.
4. Addressing the Posterior Longitudinal Ligament
- The posterior longitudinal ligament (located in front of the spinal cord) is shaved to remove hardened or buckled areas that may contribute to spinal cord compression.
5. Bone Graft Preparation
- A bone graft is harvested, typically from the fibula (the thin bone on the outer side of the lower leg) or, alternatively, from the pelvis.
- The graft is prepared to fit the length of the removed sections of vertebrae and discs.
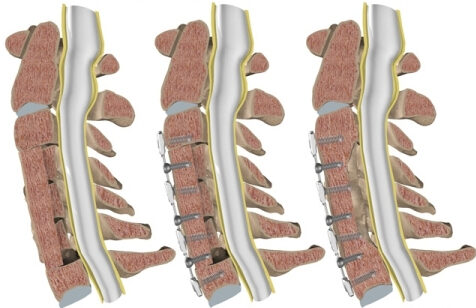
6. Graft Placement and Stabilization
- Additional traction is applied to further separate the space in the spine.
- The bone graft is inserted into the gap, acting as a supportive column (strut) to maintain spinal stability and alignment.
- A metal plate may be attached to the front of the spine to secure the graft.
- An X-ray ensures proper placement of the graft and hardware.
7. Closure and Post-Surgery Stabilization
- The muscles and soft tissues are repositioned, and the incision is stitched closed.
- Patients are typically fitted with a rigid neck brace for at least three months to keep the neck immobile while the bone graft fuses with the surrounding vertebrae.
This comprehensive procedure is designed to alleviate spinal cord compression and restore stability to the cervical spine.
Complications
Cervical corpectomy is a complex surgical procedure, and while it is generally safe, complications can arise. Below are the most common risks associated with this surgery:
Common Complications
- Anesthesia-related issues
- Thrombophlebitis (blood clots)
- Infections
- Nerve damage
- Problems with the bone graft or hardware
- Nonunion (failed fusion)
- Persistent pain
1. Problems with Anesthesia
Anesthesia may occasionally interact with other medications or cause rare adverse effects. Possible concerns include:
- Lung function suppression during surgery due to reduced lung expansion.
- Allergic or unexpected reactions to anesthetics.
Preventative Measure:
Discuss potential anesthesia risks with your anesthesiologist prior to the procedure.
2. Thrombophlebitis (Blood Clots)
Deep venous thrombosis (DVT) can occur after any surgery, where blood clots form in the large veins of the leg. If a clot travels to the lungs, it can result in a pulmonary embolism, a potentially life-threatening condition.
Preventative Steps:
- Early mobilization after surgery.
- Use of pressure stockings to keep blood flow steady.
- Administration of blood-thinning medications to prevent clot formation.
3. Infection
Infections, though rare, can occur:
- Superficial infections of the skin can be treated with antibiotics.
- Deep infections involving bones or tissues may require further surgical intervention.
Antibiotics are often administered before surgery to minimize infection risks, especially when using bone grafts or hardware.
4. Nerve Damage
Surgeries near the spinal canal carry a risk of:
- Direct injury to nerves or the spinal cord, leading to muscle weakness or numbness.
- Damage to the nerve connected to the voice box, potentially causing temporary or, in rare cases, long-term hoarseness or voice fatigue.
Preventative Measure:
Surgeons often approach the spine from the left side of the neck, where nerve pathways are more predictable.
5. Graft or Hardware Problems
The bone graft or implanted hardware may cause complications:
- The graft could shift out of position, requiring additional surgery to secure it.
- Hardware, such as plates or screws, might loosen or break, irritating surrounding tissues.
Potential Solution:
A second surgery might be necessary to fix or replace problematic hardware or grafts.
6. Nonunion (Failed Fusion)
Sometimes, the vertebrae fail to fuse together properly, resulting in a nonunion (pseudarthrosis). This can cause ongoing joint motion and pain.
Management:
A second surgery may involve additional bone grafting and hardware placement to promote successful fusion.
7. Persistent Pain
Although cervical corpectomy relieves spinal cord compression, not all patients experience complete pain relief. Residual or new pain may occur due to:
- Remaining spinal conditions.
- Scar tissue formation.
Next Steps:
Discuss persistent symptoms with your surgeon to explore pain management options.
Summary
While cervical corpectomy is effective in treating conditions like spinal stenosis, it is important to understand the potential risks. Careful surgical planning, postoperative care, and prompt management of complications can significantly reduce risks and improve outcomes. Always communicate with your surgeon about any concerns before and after surgery.
After Surgery: What to Expect
Following a cervical corpectomy, recovery involves a combination of protective measures, physical therapy, and gradual resumption of activities to ensure proper healing.
Postoperative Care
- Neck Immobilization:
- Most patients are fitted with a rigid neck brace or a halo vest for at least three months to stabilize the neck and protect the surgical site.
- If metal hardware was attached during surgery, these restrictive measures may not be necessary.
- Hospital Stay:
- The average hospital stay lasts up to one week after the procedure.
- During this time, a physical therapist will guide patients on safe movement techniques, such as how to:
- Transition in and out of bed.
- Dress and perform daily tasks without stressing the neck.
Returning Home
- Activity Restrictions:
- Patients are advised to limit physical activity to promote graft healing and prevent strain on the neck.
- Heavy lifting, bending, or twisting should be avoided during the initial recovery phase.
- Physical Therapy:
- Outpatient physical therapy typically begins around five weeks after surgery.
- The focus is on regaining neck strength, flexibility, and safe movement patterns to support long-term recovery.
Healing Timeline
- The initial months post-surgery are critical for the bone graft to heal and fuse. Patients are encouraged to follow their surgeon’s recommendations closely to ensure optimal recovery outcomes.
Rehabilitation: What to Expect During Recovery
Recovering from cervical corpectomy surgery requires patience and commitment, as the process can extend over several months to a year. A combination of physical therapy, gradual return to activities, and lifestyle adjustments supports optimal recovery.
Initial Phase of Rehabilitation
- Duration:
- Physical therapy sessions typically last two to three months, with full recovery taking up to one year.
- Pain and Inflammation Management:
- Treatments:
- Ice therapy and electrical stimulation to reduce pain and swelling.
- Massage therapy and manual techniques to alleviate muscle spasms and stiffness.
- Treatments:
Progressive Active Treatments
- Cardiovascular Exercises:
- Gradual introduction of walking, stationary cycling, or arm cycling to improve heart and lung function.
- Muscle Strengthening and Control:
- Specific exercises to strengthen neck and upper back muscles for better stability and posture.
- Body Mechanics Training:
- Focus on safe movement techniques, including:
- Getting in and out of bed.
- Dressing and performing routine activities safely.
- Lifting and carrying items without straining the neck.
- Focus on safe movement techniques, including:
Return to Work and Daily Activities
- Customized Plans:
- As you recover, your therapist will design a tailored program to prepare you for returning to work.
- For physically demanding jobs, adjustments or alternate tasks may be necessary to minimize strain on the neck.
Preventive Education
- Future Problem Avoidance:
- Before concluding therapy, your therapist will teach strategies to reduce the risk of re-injury, emphasizing proper body mechanics and ergonomics in daily life.