Introduction to Calcific Tendinitis
Calcific tendinitis of the shoulder occurs when calcium deposits accumulate in the tendons of the shoulder, often leading to significant pain and inflammation in the surrounding tissues. This condition is relatively common, particularly in individuals over 40 years of age.
This guide provides insights into:
- The changes that occur in the shoulder due to calcific tendinitis.
- Diagnostic tests your doctor may use to confirm this condition.
- Effective strategies for managing and relieving shoulder pain.
Anatomy
What is Affected?
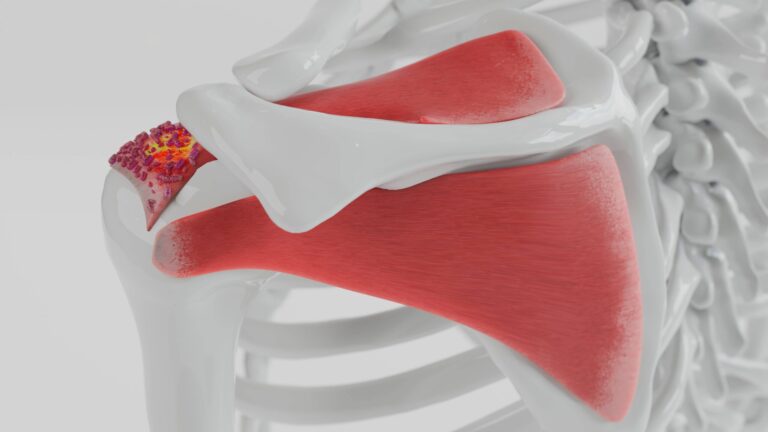
Calcific tendinitis impacts the tendons of the rotator cuff, a group of tendons connecting the shoulder muscles to the humerus (upper arm bone). Calcium deposits commonly form in the supraspinatus tendon, one of the primary tendons in the rotator cuff.
Types of Calcific Tendinitis
- Degenerative Calcification
Degenerative calcification is primarily caused by the natural wear and tear of aging. As we grow older:- Blood flow to the rotator cuff tendons decreases, weakening them.
- Continuous shoulder use causes the tendon fibers to fray, much like a worn-out rope.
- Calcium deposits form in the damaged areas as part of the body’s healing response.
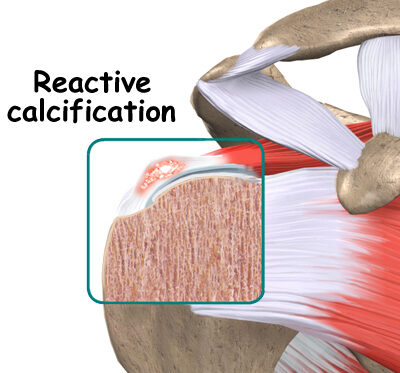
- Reactive Calcification
Reactive calcification differs in its cause and progression:- The exact trigger is unclear, but it is unrelated to degeneration.
- It is more likely to cause significant shoulder pain compared to degenerative calcification.
Stages of Reactive Calcification:
- Pre-Calcific Stage: Changes occur in the tendon, making it more prone to calcium deposits.
- Calcific Stage: Calcium crystals accumulate in the tendons and later begin to dissolve. This is the stage where pain often peaks.
- Post-Calcific Stage: The body reabsorbs the calcium deposits, heals the tendon, and remodels it with new tissue.
Understanding these stages and types of calcific tendinitis is crucial for determining the appropriate treatment plan.
Causes
The exact cause of calcific tendinitis remains uncertain. However, researchers have identified factors that may contribute to its development based on the type of calcification:
Degenerative Calcification
This form of calcific tendinitis is commonly associated with aging and tendon wear and tear. Possible contributing factors include:
- Decreased Oxygen Supply: Reduced blood flow to the tendon tissues as we age may lead to calcium deposits.
- Pressure or Damage: Repeated stress or pressure on the tendons can result in tissue damage, triggering calcium formation as part of the healing process.
Reactive Calcification
Reactive calcification is less understood and:
- Often occurs in younger individuals.
- May resolve on its own without intervention in many cases.
While the mechanisms behind reactive calcification remain unclear, it appears unrelated to the typical wear and tear seen in degenerative calcification.
By recognizing these potential causes, healthcare providers can better tailor treatment approaches to the specific type of calcific tendinitis.
Symptoms
The symptoms of calcific tendinitis can vary depending on the stage of the condition. While calcium deposits are forming, discomfort may be mild or absent. However, during the reabsorption stage, pain can intensify significantly.
Common Symptoms:
- Mild to Moderate Pain (Calcium Deposition Phase):
- Some individuals may experience mild discomfort or no pain during this stage.
- Severe Pain (Reabsorption Phase):
- Pain often peaks when calcium deposits are being reabsorbed by the body, although the exact reason is unclear.
- Stiffness and Limited Mobility:
- Shoulder stiffness may make it difficult to lift your arm or perform daily activities.
- Pain During Movement:
- Lifting the arm can be particularly painful due to inflammation in the affected tendons.
- Sleep Disruption:
- Severe pain may interfere with sleep, especially when lying on the affected shoulder.
Recognizing these symptoms early can help in seeking timely treatment, preventing further discomfort, and maintaining shoulder mobility.
Diagnosis
Diagnosing calcific tendinitis involves a combination of medical history, physical examination, and imaging tests to confirm the presence of calcium deposits and evaluate their progression.
Steps in Diagnosis
- Medical History and Physical Examination
- Your doctor will review your symptoms, medical history, and any activities that may have contributed to shoulder pain.
- A physical exam will assess the range of motion, tenderness, and severity of discomfort in your shoulder.
- Imaging Tests
- X-rays:
- X-rays are essential to detect calcium deposits and confirm their exact location in the shoulder tendons.
- These images help differentiate calcific tendinitis from other shoulder conditions that may cause similar pain.
- Repeat X-rays:
- Over time, additional X-rays may be required to monitor changes in the size and location of the calcium deposits.
- These follow-ups help your doctor assess whether the deposits are resolving naturally or if surgical intervention might be necessary.
- X-rays:
Accurate diagnosis through these steps ensures the appropriate treatment plan is developed for managing calcific tendinitis effectively.

Treatment
Managing calcific tendinitis involves both nonsurgical and advanced treatments aimed at relieving pain, reducing inflammation, and promoting healing. Your doctor’s initial focus will be to control pain and address inflammation using a stepwise approach.
Nonsurgical Treatment Approaches
- Rest and Anti-Inflammatory Medication
- Resting the affected shoulder and avoiding activities that worsen symptoms are essential.
- Over-the-counter anti-inflammatory drugs, such as ibuprofen, are often recommended to control pain.
- Cortisone Injections
- For severe, persistent pain, your doctor may administer a cortisone injection, a potent steroid that temporarily reduces inflammation and swelling.
- Lavage (Calcium Removal Procedure)
- During the reabsorption phase, when pain is typically most intense, lavage may be recommended.
- This procedure involves inserting two large needles into the affected area to flush out calcium deposits with sterile saline.
- Lavage can help:
- Break loose and remove calcium deposits.
- Alleviate pressure within the tendon, even if complete removal isn’t achieved.
Rehabilitation Therapy
Your doctor may prescribe physical or occupational therapy to aid recovery:
- Pain Relief Techniques:
- Heat or ice application to ease inflammation and discomfort.
- Ultrasound Therapy:
- Ultrasound can reduce calcium deposits, alleviate pain, and improve arm function.
- To achieve results, repeated treatments (up to 24 sessions over six weeks) are necessary.
Shock Wave Therapy
- A newer, non-invasive option that uses shock wave pulses to target the affected area.
- Typically administered once per week for up to three weeks.
- Benefits include:
- Breaking down calcium deposits for easier absorption by the body.
- Reducing pain and improving shoulder mobility, as supported by recent studies.
Conclusion
Nonsurgical treatments for calcific tendinitis, such as rest, medication, lavage, and shock wave therapy, aim to relieve pain and improve functionality. For optimal recovery, a combination of these methods, guided by medical professionals, can help manage symptoms and accelerate healing effectively.
Surgical
When nonsurgical treatments fail to relieve pain or restore shoulder movement, and the condition significantly impacts daily life, surgery may be required. Surgical procedures for calcific tendinitis are typically outpatient, meaning patients can return home the same day. These surgeries involve the use of anesthesia.
Arthroscopic Resection
This is the most common surgical approach for calcific tendinitis and involves minimally invasive techniques:
- Procedure:
- A small camera, called an arthroscope, is inserted into the shoulder joint through a tiny incision.
- Additional small incisions are made to insert surgical tools.
- Steps:
- The arthroscope helps the surgeon locate calcium deposits within the rotator cuff tendon.
- Small instruments are used to resect (remove) the deposits.
- The area is thoroughly rinsed to eliminate loose calcium crystals that could irritate surrounding tissues.
- Benefits:
- Minimally invasive with shorter recovery times.
- Reduced pain and scarring compared to open surgery.
Open Resection
Open surgery is rarely needed and reserved for severe or complex cases:
- Procedure:
- The surgeon makes a larger incision to access the shoulder.
- Surrounding muscles and tissues are carefully cut to expose the tendon.
- The calcium deposits are removed, and the area is rinsed to clear any remaining calcium crystals.
- Post-Surgery:
- The surgeon repairs the tendon and closes the incision with sutures.
- Considerations:
- Longer recovery period due to the more invasive nature of the procedure.
- Recommended only when arthroscopic surgery is not feasible.
Conclusion
Surgical options, particularly arthroscopic resection, are effective in treating calcific tendinitis when nonsurgical treatments prove inadequate. These procedures aim to remove calcium deposits, alleviate pain, and restore mobility, helping patients return to their normal activities. Open surgery, while less common, offers an alternative for more severe cases.
Rehabilitation After Calcific Tendinitis Treatment: What to Expect
Rehabilitation is a crucial part of recovery from calcific tendinitis, whether you undergo nonsurgical treatment or surgery. A structured rehabilitation plan focuses on restoring strength, improving range of motion, and preventing future issues.
Nonsurgical Rehabilitation
Even without surgery, a rehabilitation program may be necessary to strengthen and stretch the shoulder:
- Therapist-Guided Exercises:
- A physical or occupational therapist may create a personalized program lasting four to six weeks.
- Exercises focus on strengthening the rotator cuff muscles, which stabilize the shoulder joint.
- Benefits of Strengthening:
- Strengthening the rotator cuff muscles reduces pressure on calcium deposits, alleviating discomfort.
- Ergonomic Adjustments:
- Therapists can evaluate your workstation or daily activities and recommend posture or movement changes to prevent further problems.
Post-Surgery Rehabilitation
Recovery after shoulder surgery requires a gradual and carefully managed rehabilitation plan:
Initial Recovery Phase (0-2 Weeks):
- Support:
- A sling may be used for the first few days to protect the shoulder.
- Pain and Swelling Management:
- Ice packs, electrical stimulation, and gentle massage can help control post-surgical discomfort.
Rehabilitation After Arthroscopic Surgery:
- Early Exercises:
- Therapy begins quickly with range-of-motion exercises.
- Active stretching and strengthening exercises are introduced gradually.
- Caution:
- Avoid overloading the shoulder to protect healing tissues.
Rehabilitation After Open Surgery:
- Delayed Start:
- Therapy begins two to three weeks post-surgery, starting with passive exercises.
- Passive exercises involve the therapist moving the shoulder joint while keeping your muscles relaxed.
- Active Therapy:
- Begins four to six weeks after surgery, starting with isometric strengthening exercises.
- Progressive Strengthening:
- By six weeks, heavier strengthening exercises focus on improving rotator cuff and shoulder blade muscle control.
Long-Term Rehabilitation Goals
- Functional Strength:
- Exercises mimic work tasks or sports activities to prepare the shoulder for real-world movements.
- Injury Prevention:
- Your therapist will teach techniques to avoid future shoulder issues, such as proper movement patterns and posture adjustments.
Timeline for Full Recovery
- Arthroscopic Surgery:
- Therapy lasts six to eight weeks; full recovery takes about three months.
- Open Surgery:
- Recovery is slower, with full rehabilitation taking three to four months.
Conclusion
Rehabilitation is essential for achieving full recovery and preventing recurrence of calcific tendinitis. Whether through nonsurgical therapy or post-surgical rehabilitation, a structured plan focusing on strength, flexibility, and injury prevention ensures the best outcomes for long-term shoulder health.