Base of Thumb Fractures
Case
35 year old male comes in after a fall whilst playing contact sport. He has pain and deformity to the thumb with gross swelling and bruising.
Summary
Thumb function constitutes 50% of overall hand function. Recognition, early diagnosis and treatment generally result in better functional outcomes after thumb injuries. 80% of thumb fractures involve the base of the thumb or metacarpal. The 1st metacarpal is the most commonly injured as it has no protection from adjacent bones and less stability.
Presentation
- History
- Usually caused by an injury involving an axial force applied to the thumb whilst it is flexed.
- In the younger age this is usually a sports injury or road traffic accident.
- In the older age-group (>50 years) the injury is usually an accidental fall.
- Immediate pain, swelling, bruising and limitation of movement following injury
- Delayed presentations
- Hyperextension deformity may be present with a history more in keeping with base of thumb osteoarthritis.
- Swelling and bruising may have resolved with reduction in pain and partial restoration of function.
Examination
- Look
- Localised swelling and bruising
- Deformity or asymmetry
- Look for any skin breaches suggestive of open fracture (High risk of infection)
- Feel
- Localised tenderness over base of thumb
- Check neurovascular status (thumb tip pink, warm, CRT<2s, sensation to light touch)
- Move
- Pain limiting ROM
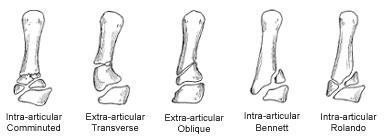
Figure1:
Red Flags:
Skin overlying the fracture
compromised = OPEN fracture
Investigation
- Imaging
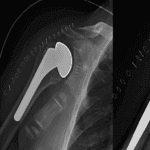
- X-ray Hand/Thumb (PA/Lateral/Oblique views)(Figure 1)
- CT Thumb
- Not routinely performed, useful to confirm joint subluxation or for pre-operative planning
- Not typically available to primary care clinicians
- MRI shoulder
- Not routinely performed, useful if associated soft tissue injury suspected
- Not typically available to primary care clinicians
Differentials
- Soft tissue injury
Classification
Based on fracture pattern (Figure 2)
- Extra-articular (Figure 1a and b)
- Oblique
- Transverse
- Intra-articular
- Bennett (Figure 1c and d)
- Rolando (Figure 1e)
- Comminuted
Extra-articular Fracture
- Usually at meta-diaphyseal junction
- Flexor pollicis longus tends to pull the distal fragment into flexion
- Abductor pollicis holds the proximal fragment in abduction
Bennett Fracture
- Fracture line into the joint surface
- Palmar ulna fragment held in place by strong anterior oblique (beak) ligament
- Abductor pollicis longus pulls shaft radially and dorsally can leave the joint subluxed/dislocated
Rolando Fracture
- Fracture line into the joint surface
- Y or T shaped fracture line
- Multiple fragments
Management
Conservative
- Closed reduction + thumb spica cast/splinting
- Elevation
- NSAIDs
- Physiotherapy after immobilisation
Operative
- Closed reduction + k-wire fixation
- Open reduction + fixation with screws or plates
- Distraction and external fixation
When to Refer
See treatment algorithm (figure 3)
Prognosis/Managing Expectations
- Immobilisation for 4-6 weeks
- Mobilisation and functional rehabilitation 3-4 months
- Incidence of post-traumatic osteoarthritis unknown but higher risk with intra-articular base of thumb fractures