Definition
The Triangular Fibrocartilage Complex (TFCC) is a crucial structure on the ulnar side of the wrist with several important roles:
- Extending the gliding surface of the radiocarpal joint
- Cushioning and stabilizing the ulnar carpus
- Stabilizing the distal radioulnar joint (DRUJ)
Injuries to the TFCC can cause ulnar-sided wrist pain, weakness, and instability, significantly impacting hand function. Proper diagnosis and treatment can restore stability, alleviate pain, and generally lead to a good prognosis for functional recovery.
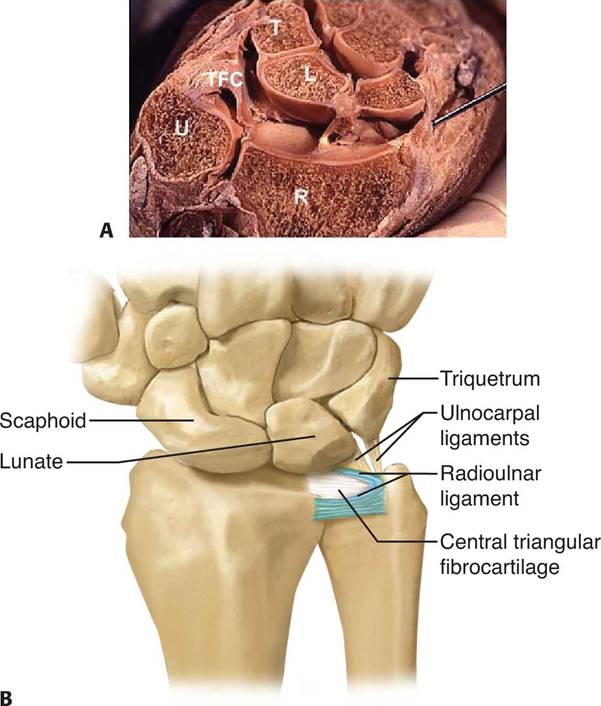
Anatomy
The TFCC consists of cartilaginous and ligamentous structures between the ulnar carpus and the distal ulna. It originates from the distal part of the sigmoid notch of the radius and inserts into the base of the ulnar styloid.
- Attachments: The TFCC connects to the ulnar carpus via the ulnocarpal ligament complex, including the ulnolunate, ulnotriquetral, and ulnar collateral ligaments.
- Stabilization: The radioulnar ligaments within the TFCC stabilize the DRUJ, limiting rotation and axial migration. The dorsal and volar radioulnar ligaments act as major stabilizers during forearm rotation.
- Structure: The central, horizontal portion of the TFCC is the thinidirectional stress.
- Vascularity: The TFCC receives blood from the ulnar artery and the dorsal and palmar branches of the anterior interosseous artery. These vessels supply the peripheral 10% to 40% of the TFCC, while the central section remains avascular, which impacts healing potential.
Biomechanics
The TFCC transmits 20% of an axially applied load from the ulnar carpus to the distal ulna. It is the primary stabilizer of the DRUJ and also stabilizes the ulna. The load on the TFCC varies with ulnar variance and forearm rotation, impacting the thickness of the central TFCC and the stability of the DRUJ.
Pathogenesis
TFCC injuries typically result from traumatic events, such as a fall on an outstretched hand or resisted torque forces. They are common in patients with neutral or positive ulnar variance and those with distal radial fractures. Degeneration of the TFCC begins in the third decade of life and increases with age, though many age-related lesions are asymptomatic.
Natural History
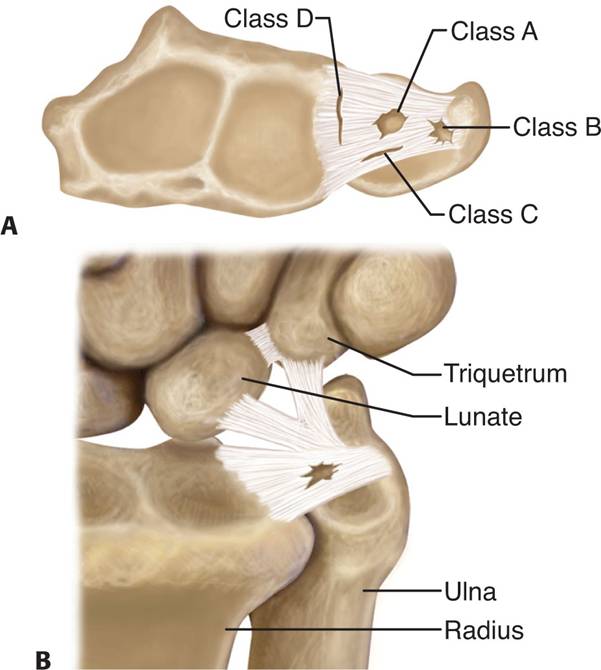
TFCC injuries are classified into traumatic and degenerative lesions, as per Palmer’s classification:
- Class 1 (Traumatic): Divided into A (central tear), B (tear from the distal ulna), C (tear from the ulnar carpus), and D (tear from the radial attachment).
- Class 2 (Degenerative): Age-related lesions characterised by central perforations and positive ulnar variance, progressing to more severe degenerative changes.
Patient History and Physical Findings
Patients with TFCC injuries typically report ulnar-sided wrist pain and clicking, often following trauma. Physical examination may reveal swelling, point tenderness over the TFCC, and signs of DRUJ instability. Additional tests include the TFCC compression test and ECU subluxation or instability examination.
Imaging and Other Diagnostic Studies
- Plain Radiographs: Essential for assessing fractures, carpal malalignment, and ulnar variance.
- MRI: Useful for diagnosing TFCC tears, especially central and radial detachments. T2-weighted images are particularly valuable.
- Arthroscopy: Considered the gold standard for diagnosing and treating TFCC lesions, providing precise information on tear location and size.
Differential Diagnosis
- ECU subluxation
- Ulnar extrinsic ligament tear
- DRUJ instability
- Triquetral avulsion fracture
- Lunatotriquetral ligament injury
- Pisotriquetral arthritis
- Ulnar artery thrombosis
- Ulnar neuropathy
- Dorsal ulnar sensory neuritis
Nonoperative Management
Initial treatment includes immobilization of the wrist and DRUJ for 4-6 weeks. Peripheral tears may heal due to their good vascularity, while central tears might become asymptomatic with immobilization. If symptoms persist, further interventions like cortisone injections may help. Class 1B lesions without ulnar styloid fractures and a stable DRUJ can also be managed nonoperatively.
Surgical Management
Patients who do not respond to nonoperative treatment require further evaluation with MRI. The specific surgical approach depends on the type of TFCC tear:
- Arthroscopic Repair: Increasingly preferred for many traumatic lesions.
- Open Repair: Sometimes necessary, particularly for radial detachments to prevent chronic DRUJ instability.
- Degenerative Lesions: Treatment may include arthroscopy and ulnar shortening osteotomy, especially for positive ulnar variance.
Proper diagnosis and timely management of TFCC injuries, whether nonoperative or surgical, are crucial for restoring wrist function and alleviating pain.