Introduction
Anterior cervical discectomy and fusion (ACDF) is a surgical procedure designed to address various neck conditions, including cervical radiculopathy, disc herniations, fractures, and spinal instability. During the procedure, the surgeon approaches the cervical spine from the front (anterior) to remove a damaged spinal disc (discectomy). The adjacent vertebrae are then stabilized using a bone graft and, in some cases, metal hardware, facilitating the fusion of the bones into a single, solid structure. This process, medically referred to as arthrodesis, aims to restore spinal stability and alleviate symptoms.
While ACDF is commonly used for these conditions, operating on the back of the neck, known as posterior cervical fusion, is more typical for treating neck fractures.
What You’ll Learn in This Guide:
- The reasons ACDF may be necessary
- The objectives surgeons aim to achieve
- What to expect during the recovery process
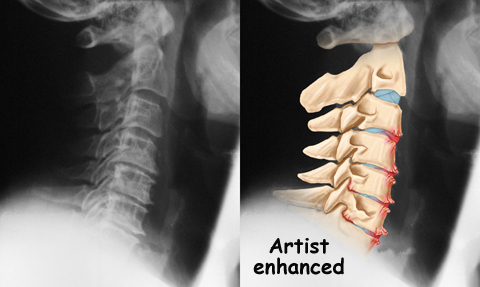
Anatomy
What Parts of the Neck Are Involved?
Anterior cervical discectomy and fusion (ACDF) is performed through the front (anterior) portion of the neck. The procedure involves several critical structures, including:
- Ligaments and Bones: These provide stability and support to the cervical spine.
- Intervertebral Discs: The soft, cushion-like structures between vertebrae that can become damaged or herniated.
- Spinal Cord and Nerves: These transmit signals between the brain and the body and may be compressed by a damaged disc.
- Neural Foramina: The openings between vertebrae through which spinal nerves exit, often affected in conditions requiring ACDF.
Rationale
What Do Surgeons Hope to Achieve with ACDF?
Anterior cervical discectomy and fusion (ACDF) is primarily performed to alleviate symptoms caused by cervical disc disease. Over time, spinal discs naturally degenerate due to aging, stress, and strain on the neck structures. This degeneration can lead to the following issues:
- Disc Collapse and Narrowed Space: As discs collapse, the space between vertebrae decreases, narrowing the neural foramina (openings where spinal nerves exit). This can compress nerves and cause pain or numbness.
- Ligament Laxity: Long spinal ligaments can slacken or buckle, putting pressure on the spinal cord.
- Disc Herniation: The outer ring of the disc (annulus) may weaken and develop cracks, allowing the central nucleus to press outward or even squeeze through. This herniation can compress spinal nerves, ligaments, or the spinal cord, leading to symptoms like pain, weakness, or numbness.
- Myelopathy: Pressure on the spinal cord can cause more severe issues, such as difficulty walking, impaired fine motor skills, and problems with bowel or bladder control.
How ACDF Resolves These Issues
- Discectomy: The damaged disc and any fragments are removed to eliminate the source of nerve or spinal cord compression.
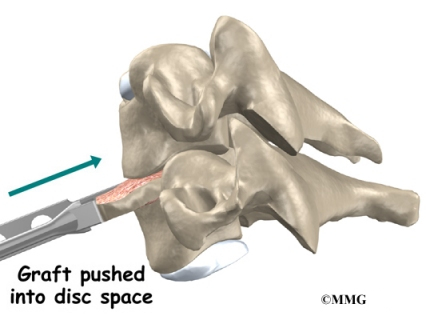
- Distraction and Bone Graft Placement: The vertebrae are gently separated (distraction) to create space for a bone graft. This can be:
- Autograft: Bone harvested from the patient’s pelvis.
- Allograft: Bone material from a donor or synthetic substitute.
The graft helps maintain the proper distance between vertebrae, widening the neural foramina and relieving pressure on nerves. Tension is also restored to slackened ligaments, preventing them from buckling into the spinal canal.
- Fusion: The graft stabilizes the vertebrae, stopping movement at the affected segment. This helps:
- Relieve pain by immobilizing the problematic area.
- Prevent further degeneration, including the formation of bone spurs.
- Allow existing bone spurs to shrink naturally.
By stabilizing the spine and alleviating nerve compression, ACDF aims to prevent future complications and eliminate ongoing pain caused by cervical disc disease.
Preparations
How Should You Prepare for ACDF Surgery?
The decision to undergo anterior cervical discectomy and fusion (ACDF) is made collaboratively between you and your surgeon. It’s essential to fully understand the procedure and address any concerns with your healthcare provider.
Before surgery, your surgeon may recommend a comprehensive physical examination with your primary care doctor to confirm you are fit for the operation.
Key Preparations Include:
- Fasting: Avoid eating or drinking after midnight on the night before surgery.
- Admission: You will likely be admitted to the hospital early on the day of your procedure.
Surgical Procedure
What Happens During ACDF Surgery?
ACDF is typically performed under general anesthesia, which ensures you are asleep and pain-free throughout the procedure. A ventilator may be used to assist with breathing.
Step-by-Step Process:
- Incision and Access:
- The surgeon makes a small incision (around 2 inches) on the left side of your neck, just above the collarbone.
- Soft tissues and muscles are gently retracted to expose the spine while avoiding the nerve to the voice box.
- Disc Removal:
- A needle and X-ray are used to confirm the affected disc.
- The disc and any herniated material pressing on nerves are removed with precision tools.
- Bone Preparation:
- The surfaces of the vertebrae are shaved to encourage bone graft healing.
- Bone graft material, either from your pelvis (autograft) or a donor (allograft), is shaped to fit snugly into the space where the disc was removed.
- Fusion and Stability:
- The vertebrae are gently separated to place the graft securely.
- Traction is released, and the graft is tested to ensure proper placement and stability. An X-ray may be taken for confirmation.
- Closure:
- A drainage tube may be inserted to prevent fluid build-up.
- Soft tissues and skin are sutured, and a neck brace may be applied to stabilize the spine during recovery.
Complications
What Risks Are Associated with ACDF Surgery?
Like all major surgical procedures, anterior cervical discectomy and fusion (ACDF) carries the risk of complications. The most common issues include:
- Anesthesia-related problems
- Thrombophlebitis (blood clots)
- Infection
- Nerve damage
- Graft-related issues
- Nonunion (failure of the bones to fuse)
- Persistent or ongoing pain
This list covers the primary risks, but other rare complications may also occur.
Anesthesia-Related Problems
Complications from anesthesia can arise if it interacts with other medications the patient is taking or if the patient has a rare adverse reaction. Additionally, general anesthesia may temporarily impair lung function due to reduced expansion during the procedure. Patients are advised to discuss their medical history and concerns with the anesthesiologist before surgery.
Thrombophlebitis (Blood Clots)
Thrombophlebitis, also known as deep venous thrombosis (DVT), occurs when blood clots form in the large veins of the leg. Symptoms may include swelling, warmth, and pain in the affected leg.
If a clot travels to the lungs, it can cause a potentially life-threatening condition known as a pulmonary embolism, which blocks blood flow in the lungs.
Preventative Measures:
- Early mobility post-surgery
- Wearing pressure stockings to promote blood flow
- Taking blood-thinning medications as prescribed
Infection
While rare, infections after spine surgery can range from superficial (skin-level) to deep infections affecting bones and soft tissues.
- Superficial Infections: Often treated effectively with antibiotics.
- Deep Infections: May require additional surgery to remove infected tissue.
Nerve Damage
The proximity of the spinal cord and nerves to the surgical site increases the risk of injury. Nerve damage can occur due to:
- Physical contact with surgical instruments
- Swelling near the nerves
- Formation of scar tissue post-surgery
Potential Symptoms:
- Muscle weakness
- Loss of sensation
- Temporary or permanent hoarseness or voice changes (if the nerve to the voice box is affected)
Surgeons typically operate on the left side of the neck to minimize risks to the nerve controlling the voice box.
Problems with the Graft
Bone grafts, commonly harvested from the pelvic rim or obtained from donors, may sometimes cause complications, such as:
- Pain or weakness at the graft site
- Infection in the grafted area
- Graft migration, which may destabilize the spine and require corrective surgery
Nonunion (Pseudarthrosis)
Nonunion occurs when the bones fail to fuse properly after surgery. This can lead to persistent pain and require a secondary operation to add more bone graft material and/or secure the area with metal plates and screws.
Ongoing Pain
While many patients experience significant relief from ACDF, some may continue to feel pain after the surgery. Persistent discomfort may result from:
- Incomplete relief of nerve compression
- Scar tissue formation
- Nonunion or other postoperative complications
Patients experiencing prolonged or severe pain should consult their surgeon for appropriate management options.





