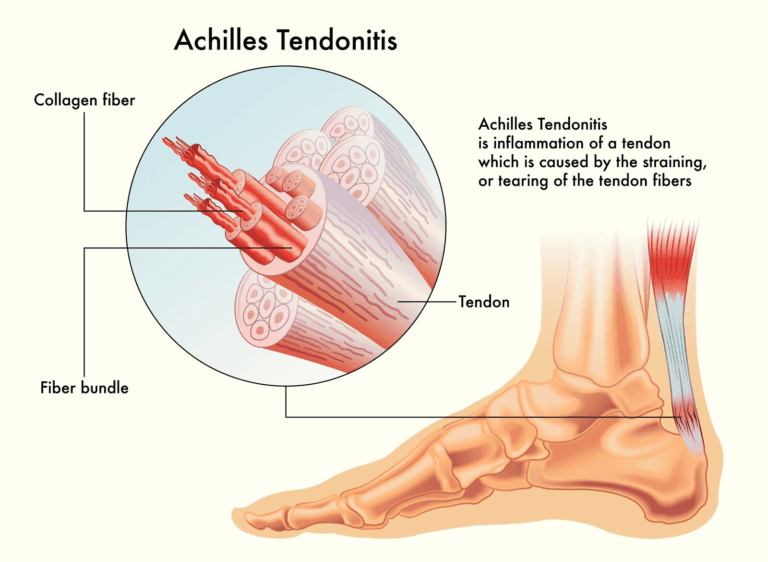
Achilles tendonitis is a prevalent condition characterised by irritation and inflammation of the large tendon running down the back of the lower leg. The Achilles tendon is the largest in the body, connecting the calf muscles to the heel bone. It plays a crucial role in walking, running, climbing stairs, jumping, and standing on tiptoes.
Despite its ability to withstand significant stress from these activities, it is prone to tendonitis, often due to overuse.
Anatomy and Types of Achilles Tendinitis

Achilles tendinitis pain can manifest within the tendon itself or at the point where it attaches to the heel bone, known as the Achilles tendon insertion.
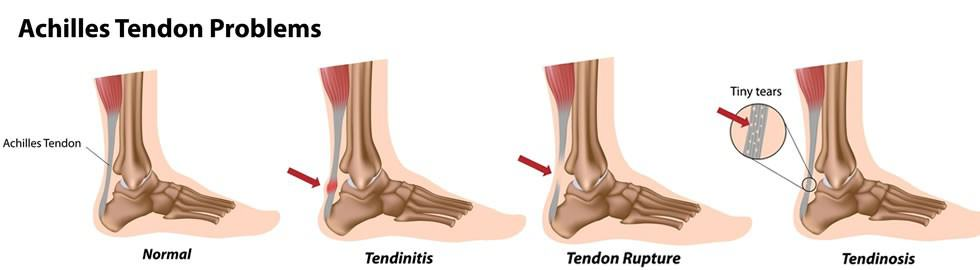
Tendinitis, or tendonitis, is acute tendon inflammation that causes swelling, pain, and irritation. Chronic tendon damage can lead to tendinopathy, which includes tendinitis and tendinosis. Unlike an Achilles tendon rupture, which involves a sudden tear or separation from the heel bone, Achilles tendinitis develops gradually due to repetitive stress.
There are two types of Achilles tendinitis:
- Noninsertional Achilles Tendinitis:This affects the middle portion of the tendon above where it attaches to the heel. Over time, the tendon fibres may break down, leading to tiny tears, swelling, and thickening. This type is more common in younger, active individuals, especially runners.
- Insertional Achilles Tendinitis: This involves the lower portion of the tendon, where it inserts into the heel bone (calcaneus). Damaged tendon fibres may calcify over time, and bone spurs often form on the heel. This type can occur at any age or activity level but is also most common in runners and is usually caused by tight calf muscles, which increase stress on the tendon.
Causes and Risk Factors
Achilles tendinitis is typically not linked to a specific injury but results from repetitive stress. Factors contributing to its development include:
- A sudden increase in exercise intensity or duration without proper adjustment.
- Tight calf muscles, which place extra stress on the Achilles tendon.
- Haglund’s deformity is an abnormal bone growth on the back of the heel that can irritate the tendon.
Symptoms
Common symptoms of Achilles tendinitis include:
- Pain and stiffness along the tendon, especially in the morning.
- Pain that worsens with activity or the day after exercising.
- Thickening of the tendon.
- Bone spur formation in insertional tendinitis.
- Swelling increases with activity.
- Heel pain when wearing shoes.
If you experience a sudden pop in your calf or heel, seek immediate medical attention, as this may indicate a tendon tear.
Diagnosis
A doctor will examine your foot and ankle, looking for swelling, bone spurs, pain along the tendon, and limited range of motion. Imaging tests like X-rays, MRI, and ultrasound can help determine the severity of the condition and guide treatment planning.
Treatment
Most cases of Achilles tendinitis respond well to nonsurgical treatment, although full recovery may take several months. Critical nonsurgical treatments include:
- Rest: Reducing or stopping activities that worsen the pain. Switching to low-impact activities like biking, swimming, or using an elliptical can help.
- Ice: Applying ice to the painful area for up to 20 minutes can reduce pain and swelling.
- NSAIDs:Non-steroidal anti-inflammatory drugs like ibuprofen and naproxen can help manage pain and swelling, allowing physical therapy exercises.
- Physical Therapy:Exercises to strengthen the calf muscles and improve flexibility can aid recovery.
- Orthotics and Proper Footwear: Using supportive shoes or orthotics to reduce stress on the tendon.
- Ankle Brace or Boot: In some cases, immobilisation with an ankle brace or boot may be recommended.
In severe cases where nonsurgical treatments are ineffective, surgery may be considered to repair the damaged tendon.
Achilles tendinitis requires careful management to prevent recurrence. Gradual increase in activity levels, proper warm-up and cool-down exercises, and maintaining flexibility and strength in the calf muscles are essential preventive measures.
Physiotherapy
Physical therapy is very helpful in treating Achilles tendinitis. The following exercises and stretches can help to strengthen the calf muscles and reduce stress on the Achilles tendon.
- Calf Stretch:
Lean forward against a wall with one knee straight and your heel on the ground. Place the other leg in front, with the knee bent. Push your hips toward the wall to stretch the calf muscles and the heel cord. Hold for 10 seconds and relax. Repeat 20 times for each foot.
- Eccentric Strengthening: Contracting a muscle while it lengthens. Perform under supervision initially. Examples include:
- Bilateral Heel Drop:
Stand on a stair with just the front half of your foot on the stair. Lift your heels, then slowly lower them. Repeat 20 times.
- Single Leg Heel Drop: Similar to the bilateral heel drop but done on one leg.
Ice
Applying ice to the painful area can reduce pain and swelling. Use for up to 20 minutes at a time.
Non-steroidal Anti-inflammatory Drugs (NSAIDs)
Drugs like ibuprofen and naproxen can help manage pain and swelling.
Orthotics and Proper Footwear
Supportive shoes or orthotics can reduce tendon stress. Heel lifts can decrease strain. In severe cases, a walking boot may be recommended.
Night Splinting
Using night splints can provide significant relief for morning pain. These braces keep your foot in a stretched position overnight.
Extracorporeal Shockwave Therapy (ESWT)
ESWT uses shockwaves to promote healing. High-energy ESWT requires anaesthesia, while low-energy ESWT does not. This therapy has shown promise in reducing pain and improving function.
Cortisone Injections
Cortisone injections are not recommended for Achilles tendinitis as they can weaken the tendon and increase the risk of rupture.
Platelet-Rich Plasma (PRP) Injections
PRP injections have shown some improvement in pain, but more research is needed to confirm their effectiveness.
Surgical Treatment
Surgery is considered if pain does not improve after 6 months of nonsurgical treatment. Types of surgery include:
- Debridement: Removal of damaged tissue and bone spurs. The remaining tendon is reattached to the heel bone with anchors or stitches.
- Gastrocnemius Recession: Surgical lengthening of the calf muscles to reduce stress on the tendon.
- Minimally Invasive Surgery: Uses small incisions and instruments to remove damaged tendon tissue or release parts of the tendon and muscle from the bone.
Outcomes
Surgical outcomes are generally good, with high rates of pain reduction and improved function. Physical therapy is crucial for recovery, and full rehabilitation may take up to 12 months. Continued pain after surgery can occur in 20% to 30% of patients, and wound infections are a potential complication.
By understanding the causes, symptoms, and treatment options for Achilles tendinitis, patients can take proactive steps to manage their condition and seek appropriate medical care. Proper management and treatment can lead to significant improvements in pain and function, allowing individuals to return to their regular activities.