Each mile you walk places approximately 60 tons of pressure on your feet, making them one of the hardest-working parts of your body. While feet are designed to endure significant stress, excessive strain can push them beyond their limits, leading to discomfort and pain. Heel pain, in particular, is one of the most frequent issues people experience, often stemming from overuse or improper foot care.
Anatomy
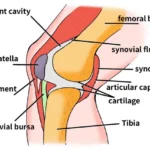
The bones in the foot are typically categorized into three sections:
- Hindfoot: The rear portion of the foot.
- Midfoot: The central section of the foot.
- Forefoot: The front part of the foot.
The heel bone (calcaneus) is the largest bone in the foot, located in the hindfoot at the back of the foot.
Two key structures are directly connected to the heel bone:
- The Achilles tendon, which stretches from the calf muscle to attach at the back of the heel.
- The plantar fascia, a thick, fibrous band of tissue running along the sole of the foot and attaching to the bottom (plantar surface) of the heel bone.
When these attachment points — where soft tissues connect to bone — become inflamed, they can cause significant heel pain.
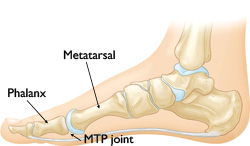 The MTP joint is the large joint closest to the base of the big toe.
The MTP joint is the large joint closest to the base of the big toe.
Causes of Heel Pain
Heel pain can arise from a variety of causes, broadly categorized into pain beneath the heel and pain behind the heel.
Pain Beneath the Heel
- Stone Bruise: Stepping on a hard object, such as a rock, can bruise the fat pad beneath the heel. Although the area may not always show visible discoloration, the pain can be significant.
- Plantar Fasciitis: Excessive running or jumping can inflame the plantar fascia, the tissue connecting the heel bone to the base of the toes. This condition is often aggravated by wearing old or worn-out shoes lacking proper cushioning. Learn more about: Plantar Fasciitis and Bone Spurs.
- Heel Spur: If plantar fasciitis is left untreated, a heel spur — a calcium deposit — may develop where the plantar fascia connects to the heel bone. While the spur itself is rarely painful, it often results from chronic inflammation caused by untreated plantar fasciitis.
- Calcaneus Stress Fracture: High-impact activities can cause repetitive stress on the heel bone (calcaneus), leading to fractures over time. Learn more about: Stress Fractures of the Foot and Ankle.
- Nerve Entrapment: Continuous repetitive impact can cause swelling and inflammation of nerves under the heel, leading to significant pain.
Pain Behind the Heel
- Retrocalcaneal Bursitis: This condition involves inflammation at the point where the Achilles tendon attaches to the heel bone. It can result from excessive running or wearing shoes that irritate or rub against the back of the heel.
- Insertional Achilles Tendinosis: Over time, the Achilles tendon can deteriorate at its insertion point on the heel bone, leading to thickening and pain. This condition is often the result of repetitive strain or aging-related changes in the tendon.
A Word of Caution
Regardless of the underlying cause, continuing to apply pressure or impact on an already sore heel will likely exacerbate the condition, potentially leading to more severe complications. Early identification and management of the root cause are critical for effective recovery.
Symptoms of Heel Pain
Heel pain is often characterized by swelling, tenderness, and discomfort that can vary depending on the underlying cause.
Symptoms of Pain Beneath the Heel
- In cases of plantar fasciitis, the pain is typically localized under the heel and may begin as mild discomfort.
- The pain is most pronounced during the first steps of the day, such as getting out of bed in the morning or stepping out of a car after a prolonged drive.
- Extended periods of inactivity, like sitting for long durations, can also lead to a sharp flare-up of pain when standing or walking again.
Symptoms of Pain Behind the Heel
- Pain originating behind the heel often develops gradually, accompanied by thickened, reddened, and swollen skin in the affected area.
- The discomfort worsens when starting physical activity after a period of rest. Even wearing regular shoes can exacerbate the pain.
- In some cases, individuals may notice a tender, warm bump forming on the back of the heel.
- People born with this bump, commonly known as Haglund’s deformity, are at a higher risk of experiencing heel pain as they age.
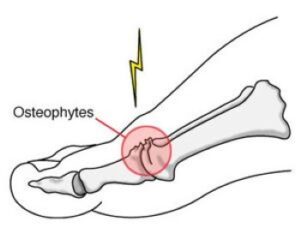
 Patients with hallux rigidus often develop a bump on the top of the foot at the base of the big toe (white arrow).
Patients with hallux rigidus often develop a bump on the top of the foot at the base of the big toe (white arrow).
General Considerations
Both types of heel pain tend to flare up with initial movement following rest but can also be aggravated by ongoing pressure or poorly fitting footwear. Early recognition of symptoms and appropriate treatment are crucial to prevent further complications.
Doctor Examination and Treatment for Heel Pain
Medical History and Physical Examination
During a consultation for heel pain, your doctor will perform a comprehensive evaluation to identify the underlying cause. This process typically includes:
- Symptom Assessment: Discussing your symptoms, such as the location, duration, and severity of the pain.
- Physical Examination: Checking the heel for signs of tenderness, swelling, or other abnormalities associated with conditions like plantar fasciitis or retrocalcaneal bursitis.
- Diagnostic Maneuvers: Squeezing the heel to detect stress fractures or asking you to perform tasks like walking or standing on one foot to assess pain triggers and pinpoint the cause.
- Range of Motion Tests: Evaluating flexibility and motion in the foot and ankle.
Imaging Tests
If the initial evaluation doesn’t yield a clear diagnosis or if the pain persists, your doctor may order imaging tests:
- X-rays: Used to identify issues like plantar fasciitis, calcaneus stress fractures, or Achilles tendinosis.
- MRI Scans: Rarely needed but can help diagnose soft tissue injuries or more complex conditions when X-rays are inconclusive and nonsurgical treatments fail.
X-ray of the feet of patient with hallux rigidus. Note the advanced arthritic changes, with large bone spurs and severe joint space narrowing in the left foot (white arrow) and the small spurs with a preserved joint space (white arrowheads) in the right foot.
Treatment Options for Hallux Rigidus
Nonsurgical Treatments
For many patients, nonsurgical interventions can effectively manage symptoms and provide relief from pain and inflammation.
Over-the-Counter Medications
- Doctors may recommend pain relievers, such as oral or topical non-steroidal anti-inflammatory drugs (NSAIDs), to alleviate discomfort and reduce swelling in the affected toe.
Ice Therapy
- Applying ice packs to the affected toe can temporarily ease inflammation and help control symptoms.
- Ensure ice is not applied directly to the skin—use a cloth or towel to avoid frostbite.
Contrast Bath Therapy
- Alternating between hot and cold water can help reduce inflammation and improve circulation.
- Use two buckets: one with cold water and the other with warm water.
- Soak the foot in cold water for 30 seconds, then switch to warm water for 30 seconds.
- Repeat the process for 5 minutes, ending with cold water.
- Perform contrast baths up to three times daily, avoiding extreme water temperatures, particularly if foot sensitivity is reduced.
- Alternating between hot and cold water can help reduce inflammation and improve circulation.
Footwear Adjustments
- Wearing shoes with a wide toe box can help reduce pressure on the big toe. High heels are discouraged.
- Shoes with stiff soles or designs like rocker bottoms may also be recommended.
- Inserts such as Morton’s extension inserts or metal plates embedded in the shoe sole can provide additional support, reduce toe bending, and alleviate pain during walking.
Corticosteroid Injections
- A corticosteroid injection into the metatarsophalangeal (MTP) joint can serve both diagnostic and therapeutic purposes.
- While the injection won’t cure the condition, it may offer pain relief for several months, particularly for patients who do not respond to other nonsurgical treatments.
Surgical Treatments
If nonsurgical options fail to relieve symptoms, surgical intervention may be necessary. The type of surgery depends on the severity of the condition and the patient’s overall health.
Cheilectomy
- Recommended for patients with mild to moderate hallux rigidus.
- Involves removing bone spurs and a portion of the big toe bone to increase the range of motion and reduce pain.
Arthrodesis
- This procedure, also known as joint fusion, is often advised for severe cartilage damage or when cheilectomy is unsuccessful.
- The surgeon removes the damaged cartilage and uses pins, screws, or plates to permanently fix the joint in place.
- While arthrodesis eliminates toe joint movement, it is the most reliable method for reducing pain and allows patients to walk comfortably. Patients may also wear low-heeled shoes post-recovery.
Final Note
Early treatment is key to managing hallux rigidus and preventing further joint damage. For most patients, nonsurgical approaches like medication, shoe modifications, and physical therapy can effectively control symptoms. However, surgical options provide reliable relief for advanced cases, particularly when nonsurgical methods are insufficient. Consulting with a healthcare professional ensures the best treatment approach tailored to individual needs.
 Arthrodesis using a plate and screws.
Arthrodesis using a plate and screws.
Arthroplasty: Joint Replacement Surgery for Hallux Rigidus
For older patients with reduced activity levels or minimal functional demands on their feet, arthroplasty (joint replacement surgery) may be an appropriate treatment option.
Procedure Overview
- During the procedure, the damaged surfaces of the metatarsophalangeal (MTP) joint are removed.
- An artificial joint is implanted to restore functionality and preserve motion.
Benefits of Arthroplasty
- Pain Relief: Replacing the joint helps alleviate discomfort caused by cartilage deterioration.
- Preservation of Mobility: Unlike arthrodesis (joint fusion), arthroplasty maintains joint motion, allowing for greater flexibility in daily activities.
Ideal Candidates
- Typically, arthroplasty is recommended for older adults or individuals who do not place high physical demands on their feet.
- It may not be suitable for highly active individuals or those with severe joint damage, as artificial joints may not withstand excessive stress over time.
Considerations
While arthroplasty can provide significant relief and improve quality of life, the procedure carries some risks, such as wear or loosening of the artificial joint over time. Discussing potential outcomes with a healthcare provider is essential to determine the best course of treatment.
 During arthroplasty, the joint surfaces are removed, and an artificial joint is implanted.
During arthroplasty, the joint surfaces are removed, and an artificial joint is implanted.