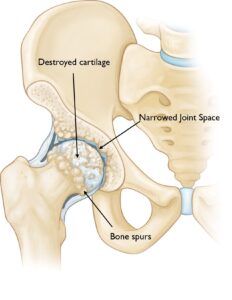
Hip osteoarthritis, often referred to as “wear-and-tear arthritis,” is a prevalent condition that typically arises with advancing age. While it can affect any joint in the body, it is most commonly found in weight-bearing joints like the hip.
This condition leads to discomfort and stiffness, making everyday tasks challenging. Simple actions such as tying your shoes, getting up from a chair, or taking a short walk may become difficult.
Since hip osteoarthritis tends to progress gradually, starting treatment early can significantly reduce its impact on your daily life. While a complete cure is not available, a variety of effective treatments can help manage pain, improve mobility, and maintain an active lifestyle.
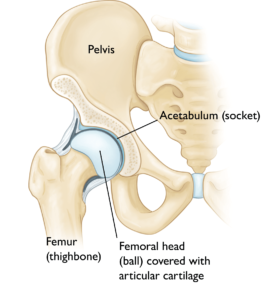
Anatomy of the Hip
The hip is one of the largest joints in the human body, functioning as a ball-and-socket joint.
The socket, known as the acetabulum, is a part of the large pelvic bone. The ball is the femoral head, located at the upper end of the femur (thighbone). Both the ball and socket are coated with articular cartilage, a smooth, slippery tissue that protects the bones, cushions impacts, and facilitates seamless movement.
A thin membrane called the synovium lines the joint’s surface. In a healthy hip, the synovium produces a small amount of lubricating fluid, which keeps the cartilage moist and aids in the joint’s mobility.