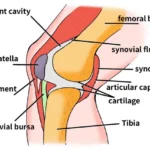
Conditions resulting in the need for arthrodesis in the hand include arthritis, unreconstructable soft tissue problems, and certain neurologic conditions.
Arthritis is the principal indication for small joint arthrodesis.
Osteoarthritis (OA) most commonly affects the DIP joints. It is estimated that at least 60% of individuals older than age 60 years have DIP joint arthritis, which may not necessarily be symptomatic.
In the early stages, the joints may be painful and swollen in spite of normal radiographs. As the arthritis progresses, osteophytes and mucous cysts may develop. Bony prominences (Heberden nodes) and angular deformities in both the coronal and sagittal planes (mallet appearance) may develop. In the final stages, DIP joint motion may be severely restricted.
OA may also involve the PIP joints and the MCP joints, especially in the index and middle fingers.
Inflammatory arthritis may also affect the small joints of the hand. About 70% of rheumatoid patients have hand involvement. Synovitis may result in deformity due to attenuation of supporting structures (collateral ligaments, extensor tendons) long before arthritic changes are evident.
At the DIP joint, terminal tendon incompetence may result in a secondary swan-neck deformity.
At the PIP joint, central slip attenuation results in a boutonnière deformity.
At the MCP joint, collateral ligament involvement may contribute to ulnar drift. Persistent synovitis produces cartilage loss.
Hand involvement in systemic lupus erythematosus (SLE) may mimic rheumatoid arthritis. Supporting structures are affected principally in SLE, which may result in joint subluxation or dislocation with relatively normal-appearing articular cartilage. The capsuloligamentous problems may compromise attempts at joint salvage.
In contrast, psoriatic arthritis may produce a remarkable degree of bone loss as the arthritis progresses. Pencil-in-cup deformity is a characteristic feature of psoriatic arthritis of the interphalangeal joints. Severe bone resorption is the characteristic feature of arthritis mutilans, most commonly seen in patients with psoriatic arthritis. Arthrodesis is the most reliable method for halting this destructive process.
Scleroderma typically produces PIP flexion and MCP extension contractures. Impaired vascularity of the digits may result in dorsal PIP ulcer formation and central slip attenuation, compounding the PIP flexion deformity.
Presentations of crystalline arthropathy in the small joints of the hand may be varied. The process may be indolent, presenting as gouty tophi over the DIP joint, or acute, presenting as an exquisitely painful, swollen, tender joint. Untreated, gout results in a resorptive arthritis.
What are the symptoms of arthritis?
The symptoms of arthritis can be:
⦁ Joint pain
⦁ Joint inflammation
⦁ Redness and heat of the skin around the joint
⦁ Decreased ability to move the joint
⦁ Joint stiffness, especially in the morning
What are the causes of arthritis?
This pathology can be a consequence of:
⦁ Bone fracture
⦁ Autoimmune disease
⦁ Infection by bacteria or viruses
⦁ Joint wear
⦁ Crystals (such as uric acid or calcium pyrophosphate dihydrate)
Can arthritis be prevented?
Joint damage can be prevented with timely and adequate diagnosis and treatment. Also, if someone has a family history it is important to talk with the doctor, even if s/he does not have any symptoms. It is also recommended to avoid repetitive and excessive movements to prevent osteoarthritis.
What is finger fusion?
A finger joint fusion for arthritis is an operation that involves removing the damaged ends of the joint, including the worn cartilage, and compressing them together until the bone has grown across the joint.
Finger fusions are often performed for osteoarthritis. The most common joint to be fused is the distal interphalangeal joint (DIP joint). This is the end finger joint, just behind the nail.
Who does it affect and why does it occur?
Finger arthritis usually occurs in patients over 40 years of age.
The articular cartilage, the slippery lining of the surface, has been worn away, and the exposed bones rub against each other, causing pain. Therefore, a small joint fusion, such as this, is very successful at reducing this pain. There are very few functional limitations as a consequence of fusing the DIP joint.
Symptoms
Patients often present with a painful, lumpy joint and a decreased range of movement.
Clinical examination
Finger arthritis usually has a stiff, swollen joint, often with knobbly bumps.
Operative treatment
here are very few non-operative treatments for DIPJ arthritis. Small splints can be worn but often get in the way, and steroid injections are quite painful and often do not work as the joint is so small and difficult to inject even with image guidance.
The surgery usually takes place under local anaesthetic, under x-ray control. A small incision is made on the back of the joint. The tendons are divided and the underlying bone exposed. The bone ends are carefully prepared by nibbling the damaged cartilage and bone and pressing the bones together. The bones are then held with various fixation devices, including buried or exposed wires, internal screws or staples. The wires are kept in place until the bone has united, usually between four and eight weeks. In contrast, the screws and staples are generally permanent implants and do not need removing unless they are causing a problem.
Fixation
There are several different fixation methods of the DIP joint, including exposed wires, buried wires under the skin, and internal screw fixation. The results of each type of surgery are very similar, and generally speaking, a 90% chance of the bones healing across can be expected. We do not use exposed wires to fuse the joints in normal circumstances as they can be awkward for patients and worry about knocking them. There is also an increased risk of infection using exposed wires.
We prefer to use internal metalwork, either screws or staples. However, a predetermined flexion can be introduced to mimic normal finger DIP posture using an internal memory stable such as the Stryker X fuse.
Post-operative rehabilitation
The skin is stitched with absorbable stitches and the wound is covered and finger protected with a small Plaster of Paris slab.
An appointment will be made to see our hand therapist within a week for dressing removal and splint to be made.
My hand therapist will often give a small splint to protect the end of the finger for the first few weeks after surgery. The wounds need to be kept dry for 10 days until healed.
Return to activities of daily living
Once the bone has grown across the joint, a rapid return to function can be expected.
Complications
The main risk is the bones not growing together. This occurs in approximately 5-10% of cases.
The vast majority of patients undergoing this operation are happy.