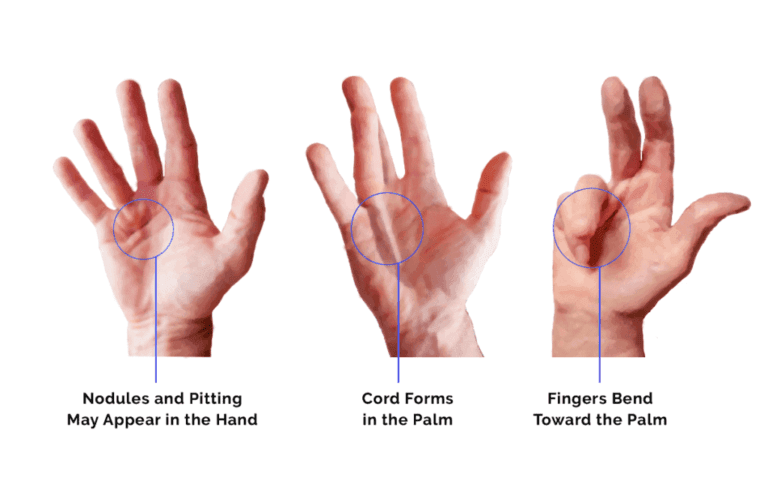
Dupuytren’s disease is a condition affecting the palmar fascia of the hand, the connective tissue beneath the skin in the palm and fingers. It ranges from small lumps or bands to thick bands, causing fingers to curl into the palm, commonly affecting the little and ring fingers and sometimes the thumb.
Cause:
The cause is unclear, but genetics may play a role. Trauma may trigger or worsen the condition in genetically predisposed individuals.
Specific demographic and health factors may increase the likelihood of developing Dupuytren’s disease:
- Age: Individuals over 50 are more susceptible to Dupuytren’s disease due to age-related changes in connective tissue.
- Family History: Genetics play a significant role, with a higher risk if a family member has the condition. Ancestral background, particularly Northern European descent, also influences susceptibility.
- Gender: Men have a greater risk and tend to experience more severe cases compared to women.
- Health Conditions: Dupuytren’s disease is associated with epilepsy and diabetes, while alcoholism and tobacco use further elevate the risk. Severity is often heightened in individuals with alcohol use disorder.
Home Remedies for Dupuytren’s Disease
While there’s no cure for Dupuytren’s contracture, you can manage symptoms and potentially slow its progression with these home remedies:
A.Relieve Palm Pressure The disease typically starts in the palm, so protecting your hands is critical:
Ease grip pressure: When gripping objects, consciously use lighter pressure to reduce strain on the affected hand.
Use gloves: Wear gloves or cushioning material, like tape, when handling tools or objects that require a firm grip to alleviate pressure on the affected hand.
B) Incorporate Exercises:
Although exercises may not halt or slow the progression of Dupuytren’s contracture, they can be beneficial, particularly in the early stages. Here are some exercises and stretches to consider:
Finger lifts:
- Place your palm flat on a smooth surface like a table.
- Lift each finger individually, pausing briefly before lowering it back down.
- Repeat several times throughout the day.
Finger spreads: Spread your fingers apart while keeping your palm flat on a surface, then bring them back together.
Palm raises: Keep your fingers flat on a surface and raise and lower only your palm.
Hand press: Place your hands together in prayer and gently push the palms and fingers against each other.
Finger bends:
- Hold your hands in front of you.
- Bend the first two joints of your fingers down.
- Straighten them.
It’s crucial to avoid overstretching, as it can exacerbate discomfort. If contracture has already begun, gently use your other hand to push the affected fingers back straight, holding for a few seconds.
Establish a routine and perform these stretches multiple times daily.
While gripping objects with excessive pressure is not advisable, practising gripping motions can help maintain grip strength and hand dexterity.
Experiment with picking up objects of varying sizes and shapes and consider gripping something soft, such as a towel, to retain grasping abilities.
C) Explore Massage Therapy:
Massage therapy can complement exercises and also serve as a standalone treatment.
Using your unaffected hand, you can gently massage your entire hand, including the palm and fingers. Alternatively, seek assistance from a family member or friend.
Be mindful to apply gentle pressure while massaging the hand. Begin by rubbing the area encompassing the thickened palm tissue, gradually moving towards the fingers.
Consider consulting a massage therapist experienced in treating Dupuytren’s disease for additional support.
It’s advisable to start massage therapy early in the progression of the condition, as it may be less effective in advanced stages.
Massage sessions may incorporate heat therapy, oils, and lotions. Look for products containing anti-inflammatory ingredients for added benefit. Alternatively, you can soothe your hand with a warm water soak or heat pack.
D)Adopt a Nutritious Diet:
Your dietary choices can impact the symptoms associated with Dupuytren’s contracture, especially if you’re middle-aged or have conditions like diabetes, which is found in approximately 5% of affected individuals.
Incorporate healthy eating habits into your lifestyle, as advised by your doctor. While adjusting may take time, maintaining a nutritious diet can become a routine part of your daily life.
Here are some guidelines to consider:
Mind portion sizes: Opt for reasonable portions, paying attention to your body’s fullness cues.
Choose whole and fresh foods:
- Prioritise whole and fresh options over processed ones.
- Select fresh vegetables over canned varieties and fresh fruit instead of canned fruit cocktails.
- Embrace whole grains to eliminate unhealthy additives like sugars and preservatives.
Limit fat intake:
- Opt for lower-fat alternatives to your favourite foods.
- Choose low-fat dairy products and lean meats such as turkey burgers instead of beef.
- Experiment with lean protein sources like chicken breast or fish.
Incorporate anti-inflammatory foods: Consider including foods known for their anti-inflammatory properties, such as green leafy vegetables, fatty fish, fruits, and nuts, in your diet.
Be mindful of potential trigger foods: Certain foods may exacerbate symptoms. As part of a balanced diet, aim to minimise processed foods and those high in salt, artificial sweeteners, and additives.
By making these dietary adjustments, you can support your overall health and potentially alleviate symptoms associated with Dupuytren’s contracture.
E )Quit Smoking and Limit Alcohol Consumption:

One of the factors that exacerbates Dupuytren’s contracture is tobacco use, as research has established a significant association between smoking and the condition. Smoking can lead to microvascular impairment, potentially contributing to the development of Dupuytren’s contracture.
Early cessation of smoking is crucial in managing the progression of the disease. Quitting smoking offers numerous health benefits, including:
- Reducing the risk of various cancers
- Improving lung and cardiovascular function
- Lowering the risk of diabetes, which is linked to Dupuytren’s disease
Additionally, heavy alcohol consumption is associated with an increased risk of Dupuytren’s contracture. While moderate alcohol intake is unlikely to impact your risk, excessive drinking can elevate it and lead to other health issues such as high blood pressure and liver damage. Consider moderating your alcohol consumption to help manage the condition.
Quitting smoking and reducing alcohol intake may be challenging, and you may require external support to overcome these addictive habits. However, the potential health improvements are substantial.
F ) Incorporate Supplements:
Alongside maintaining a healthy diet and lifestyle, consider integrating daily supplements into your regimen. Certain supplements have anti-inflammatory properties that may aid in managing symptoms associated with Dupuytren’s disease. While the effectiveness of these supplements is still under debate, you can discuss with your doctor about incorporating the following vitamins, minerals, and spices:
Vitamin E: As an antioxidant, Vitamin E helps protect the body’s cells from damage. While you may obtain some Vitamin E through your regular diet, supplementation may be considered to ensure adequate intake.
Zinc: Essential for overall health, zinc supports a healthy immune system and facilitates wound healing. Consider supplementation if your dietary intake needs to be increased.
Magnesium: Adequate magnesium intake is crucial for a balanced diet, as it contributes to various bodily functions. Low magnesium levels have been associated with a higher risk of diabetes, making magnesium supplementation a consideration.
Turmeric: Known for its anti-inflammatory properties, turmeric is a commonly used spice in cooking. Incorporating turmeric into your diet and taking it as a supplement may help mitigate inflammation associated with Dupuytren’s disease.
Before starting any supplements, please consult your healthcare provider to determine appropriate dosages and ensure they complement your treatment plan.
Professional Treatment for Dupuytren’s Disease
Injections:
Primary treatments for Dupuytren’s disease often involve minimally invasive approaches. Your healthcare provider might recommend injections as part of your treatment plan. While Dupuytren’s disease typically manifests without pain, some individuals may experience discomfort in the nodules of tissue forming in the palm.
You may be eligible for a steroid injection to reduce inflammation and pain in such cases. Multiple injections may be necessary to manage symptoms effectively.
Beyond steroid injections, other injection therapies are available for individuals with Dupuytren’s disease. Collagenase injections, for instance, can be beneficial.
Collagenase is an enzyme designed to break down collagen, the sturdy protein constituting much of our connective tissue. This enzyme is injected directly into the cords in the hand to target collagen breakdown, thereby alleviating contracture.
Following injection, typically the next day, your healthcare provider may manually manipulate the finger to break down tissue further and facilitate finger straightening.
These injections are FDA-approved and similar to steroid injections, multiple treatment courses may be required.
2. Needling:
Needle aponeurotomy, also known as needling or percutaneous needle fasciotomy, presents another minimally invasive option for treating Dupuytren’s disease.
This procedure can be performed in a clinical setting and involves inserting a needle into the tough tissue, causing finger contracture. Before the procedure, your hand will be numbed.
During needling, the needle is used to puncture the affected tissue in the hand, aiming to separate it.
Manual manipulation follows to aid in straightening the affected fingers. Additionally, a steroid injection may be administered post-needling to reduce swelling.
After the needling procedure, expect a few days of swelling and soreness, which can be managed with ice packs. While the treated hand can be used for minor activities like eating, full hand function may take one to two weeks to restore.
Your healthcare provider might recommend wearing a brace on the affected hand post-procedure. Typically, therapy is not required following a needling procedure.
3.Surgical Intervention:
In the advanced stages of Dupuytren’s disease, surgery may become necessary. When the condition progresses to severe contracture, making hand usage challenging, less invasive treatments may no longer suffice. Surgical intervention entails making an incision and excising the affected tissue.
Although surgery is more invasive, it offers a longer-term solution by releasing contracture.
Following tissue removal, incisions are sutured closed by your surgeon. Post-surgery therapy may be recommended to aid in recovery and enhance the procedure’s long-term effectiveness. Additionally, splints and bandages may be prescribed for use post-surgery. The duration of your recovery depends on the disease severity and surgical extent.
In cases of severe Dupuytren’s disease, revision surgery might be necessary. Initial surgery removes affected tissue but doesn’t address the underlying cause, leading to possible recurrence. Revision surgery targets recurring collagen-causing contracture, although it’s complex because of the presence of scar tissue.
Opting for surgery or minimally invasive treatments doesn’t preclude the use of home remedies.
Maintaining a healthy diet and taking specific supplements can bolster overall health and potentially slow disease progression.
While a definitive cure for Dupuytren’s disease remains elusive, diligent symptom monitoring, experimentation with home remedies, and seeking assistance when needed are essential aspects of managing the condition.
Post-Surgery Activities:
After surgery, the hand will be wrapped in a bulky dressing to protect it. Keeping your hand elevated is crucial to manage post-surgical swelling. Stitches are typically removed within 10 to 14 days.
Subsequently, you will commence Occupational Therapy/Physiotherapy.
It may take 6 to 12 weeks to restore your hand’s functionality fully.
During therapy sessions, your therapist will guide you through scar massage techniques and strategies to reduce swelling and improve desensitisation.
You will also engage in tailored exercises to promote recovery.
Your therapist may custom-make a thermoplastic splint for you to wear at night. Wearing the splint helps prevent the formation of contractures from surgical scars.
While you may experience stiffness in your hand in the morning, consistent use of the splint and therapeutic exercises will alleviate this over time.
During the initial weeks post-surgery, limit activities to light tasks like meal preparation, writing, and typing.
Avoid heavy lifting or activities requiring a firm grip. Recovery to full-hand use may take 6-12 weeks.
Exercise Instructions:
Stage 1:
What to Do:
- Wear your splint continuously, removing it every hour to perform hand exercises.
- Curl your fingers into the palm and hold them for 5 seconds, then straighten them and keep them for another 5 seconds. Repeat this sequence five times.
- Keep your hand elevated.
- Regularly lift your arm above your head.
- Perform elbow bending and straightening exercises regularly.
Preventing Infection:
- Frequent hand decontamination for 20 seconds using soap and water or alcohol gel.
- Refrain from visiting healthcare facilities if experiencing symptoms like diarrhoea, vomiting, cough, respiratory issues, fever, or loss of taste/smell. Seek advice from 111 instead.
- Maintain a clean and tidy environment to prevent infections in hospitals and care homes.
What Not to Do:
- Avoid using the hand for activities that may increase the risk of infection, such as gardening or dusty work.
- If the splint causes severe pain or soreness, remove it and contact your therapist.
Stage 2:
- Wear the splint only at night.
- Perform the prescribed exercises a specific number of times every few hours.
- Begin each morning with hand exercises in warm water, using a soft baby sponge if the wound is not fully healed.
Step 1:
Squeeze the sponge firmly with your fingers and maintain this position for 5 seconds.

Step 2:
Flatten the sponge using both your Palm and fingers.
The Palm of your hand. Aim to reach the base of your little finger with the tip of your thumb.

Step 3:
Maintain your fingers and wrist straight, then use your thumb to press the sponge down into the palm of your hand. Aim to reach the base of your little finger with the tip of your thumb.
Step 4:
Hold the sponge with your fingers and lift your wrist upward, holding for 5 seconds. Then, lower your wrist down and hold for another 5 seconds. Finally, pat your hand dry with a towel.

Step 5:
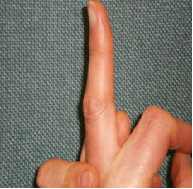
With the opposite hand, stabilise the finger just below its top joint using your thumb and fingers. Bend only the top joint, holding the position for 5-10 seconds. Repeat this for each finger.

Step 6:
Using the thumb and fingers of the opposite hand, stabilise the finger just below its middle joint. Bend only the middle joint, holding the position for 5-10 seconds. Repeat for each finger.
Step 7:
Secure the hand with the thumb of your other hand. Bend the bottom joints of your fingers while keeping the top two joints straight. Hold this position for 5-10 seconds.
Step 8:
Form a full fist, press your fingers into the fist with your other hand and squeeze tightly for 5-10 seconds. Before releasing, tense up the muscles in your forearm to maintain the tight fist for an additional 5 seconds.
After completing the exercises, massage a non-scented hand cream firmly into your scar using your thumb.
Precautions and Side Effects:
If any of the exercises cause pain, it’s essential to stop and consult with your therapist
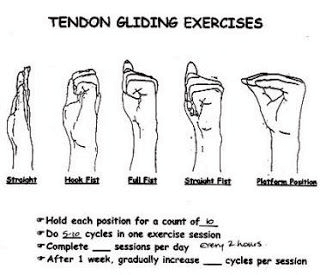
Exercises Tendon gliding exercises

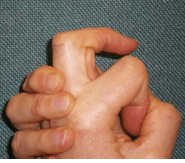
Blocked extension exercises
A

B)

C)

D)
Using your opposite hand and thumb, stabilise the bottom joint (knuckles) of your finger at a 90-degree angle.
Attempt to straighten the middle joint of your finger by blocking it with your thumb and finger, then endeavour to straighten the end joint of your finger.
Passive Flexion:
With your opposite hand, gently guide each of your fingers inward to form a fist.
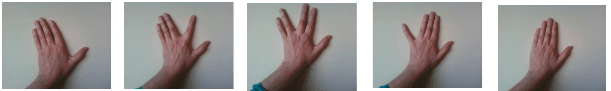
Finger Walking
Perform Finger Walking (Spreading the fingers) by resting your palm on a flat surface, moving the thumb to the side, and sliding one finger at a time toward the thumb.
Finger flexibility training
Roll a golf ball or ping pong ball between your fingers

Driving:
Before driving, inform your insurance company of recent surgery. Resume driving when you have sufficient movement and strength comfortably.
Therapy:
After surgery, keep your hand elevated to control swelling. Stitches are removed after 10-14 days, followed by Occupational Therapy/Physiotherapy. Therapy focuses on scar massage, swelling reduction, desensitisation, and exercise. A thermoplastic splint may be provided to wear at night for 4-6 months to prevent scar contraction and promote hand mobility.