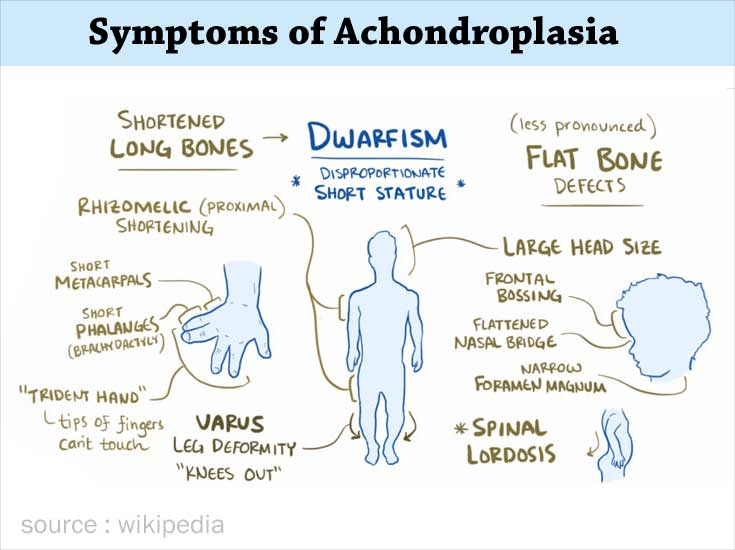
Achondroplasia is a genetic bone condition characterised by dwarfism. Infants born with achondroplasia typically exhibit shortened arms and legs, an enlarged head, and an average-sized torso. Their stature is notably shorter due to skeletal abnormalities.
The onset of achondroplasia occurs in early fetal development, wherein a genetic mutation disrupts the standard conversion of cartilage into bone. This disorder is rare, affecting approximately 1 in 10,000 newborns.
Although the likelihood of inheriting the condition increases if a parent has achondroplasia, the majority of infants born with achondroplasia have parents of average height.
Children with achondroplasia often experience health challenges, but with regular medical monitoring and intervention, many of these issues can be identified early and effectively managed. Despite these challenges, most individuals with achondroplasia can enjoy fulfilling and active lifestyles.
Description:
During early fetal development, much of the skeleton comprises a resilient and pliable tissue known as cartilage. As the fetus progresses, this cartilage undergoes ossification to form bone.
During early fetal development, much of the skeleton comprises a resilient and pliable tissue known as cartilage
Consequently, this leads to shortened bones, resulting in a distinctively short stature and other characteristic physical features.
Given that these alterations occur late in pregnancy, the condition often goes unnoticed by both doctors and parents until birth.
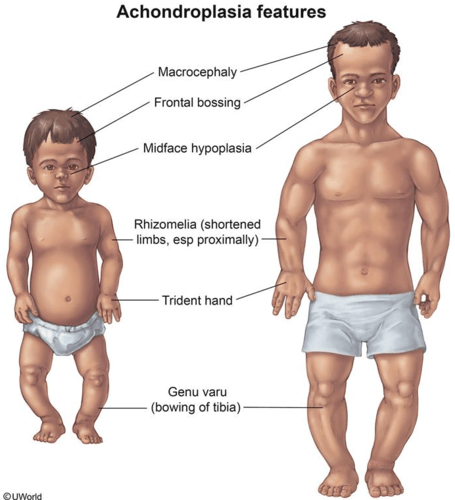
Physical Characteristics:
The physical attributes associated with achondroplasia typically manifest at birth or during infancy.
These may encompass:
- Enlarged head size with a prominent forehead
- A flattened nasal bridge and diminutive facial features
- Shortened arms and legs, with notably abbreviated upper arms and thighs
- The curvature of the lower legs
- A trunk size that generally approximates the average
- Reduced muscle tone and laxity in the joints
Other Characteristics
Early on, children with achondroplasia may delay developing some motor skills. This means they may be older than the average child when they can sit or walk alone.
Children with achondroplasia do not typically have intellectual disability. Children and adults with the condition almost always have average intelligence.
Cause:
Achondroplasia arises from a mutation in a gene crucial for skeletal growth and development.
Achondroplasia can be inherited in an autosomal dominant manner, wherein the presence of the gene mutation from a single parent is sufficient for the child to inherit the disorder. While it’s common for a parent with achondroplasia to have an affected child, with a 50% likelihood of passing on the gene, the majority of infants with achondroplasia are born to parents of average height. Surprisingly, over 80% of achondroplasia cases occur due to a spontaneous, new (de novo) mutation in the responsible gene.
At what age can achondroplasia be identified?
Achondroplasia can be detected prenatally using ultrasounds if your baby exhibits shorter-than-average limbs and a large head. However, most cases are confirmed postnatally.
How is achondroplasia diagnosed?
Diagnosis typically involves:
clinical examination.
X-rays.
Prenatal screening (if one or both parents are affected).
Genetic testing (FGFR3 gene).
MRI or CT scan to assess muscle weakness or spinal cord compression.
Treatment Approach
Clinical Examination:
Achondroplasia is occasionally identified prenatally through a prenatal ultrasound. In such cases, consulting with a pediatric orthopaedic surgeon before the baby’s birth can offer insights into the condition’s potential impact on the baby’s health.
To confirm the diagnosis postnatally, a comprehensive medical history will be taken, followed by a clinical examination, X-rays, and other imaging modalities. Genetic testing is only occasionally necessary to verify the diagnosis.
Musculoskeletal Complications:
Babies and children with achondroplasia commonly experience musculoskeletal abnormalities affecting the spine and limbs. These issues may manifest as:
In infants affected by achondroplasia, there is frequently a constriction at the base of the skull known as the foramen magnum. This narrowing can impede the passage of the brainstem and spinal cord. This compression can result in muscle weakness and respiratory difficulties. In rare cases, it can be life-threatening.
To assess the size of the foramen magnum, your child’s doctor may request an MRI scan of the spine. If deemed necessary, you may be referred to a neurosurgeon for a decompression surgery aimed at enlarging the opening in the skull to alleviate spinal cord compression
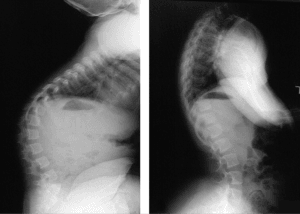
A 15-year-old girl with achondroplasia.
Spinal stenosis is a condition characterised by discomfort, numbness, and weakness in the legs. It arises when the spinal canal becomes too narrow, exerting pressure on the spinal cord and nerve roots. Due to structural differences in the vertebrae of the spine, individuals with achondroplasia, both children and adults, commonly experience spinal stenosis.
Mild symptoms of spinal stenosis can often be alleviated with weight loss, rest, pain relief medications, and adjustments in activities. However, individuals with severe symptoms may require decompression surgery to widen the space for the spinal cord and nerves. This procedure may be followed by spinal fusion surgery to stabilise the spine. In children, decompression surgery may also be followed by spinal fusion.
Kyphosis, characterised by an excessive curvature or hump in the back, is frequently observed in infants with achondroplasia due to their weak muscle tone and lax joints.
Typically, this condition resolves as the child begins walking and develops stronger core muscles.
Regular X-rays may be ordered by your child’s healthcare provider to monitor the progression of the curvature.
If the curve does not improve over time, children may need to wear a back brace to prevent further curvature or undergo corrective surgery.
The X-ray image on the left displays a kyphotic curve in the upper back of a child diagnosed with achondroplasia. On the right side, it can be observed that the curve has spontaneously corrected itself over time, a typical occurrence in children with achondroplasia.
Bowed legs, a common issue in children with achondroplasia, can lead to discomfort and difficulty walking, particularly when coupled with loose joints.
In cases of severe bowing and significant knee pain, your child’s physician may recommend one of two surgical options to correct the leg bones:
Guided growth: This procedure involves temporarily halting growth on one side of the bone and allowing the other side to catch up.
Over time, as your child grows, the bone gradually straightens.
Osteotomy: During this procedure, the curved bone is surgically cut and realigned to achieve a straightened position. The bone is stabilised during the healing process using either a plate and screws or an external fixator—a metal frame placed on the outside of the leg and secured with metal wires and pins.
Reduced elbow joint mobility is a common occurrence in children with achondroplasia, with some experiencing challenges in fully extending their elbows. Fortunately, this limitation typically does not impede daily functions.
In cases where grooming, self-care, or other routine activities become problematic, assistive tools can offer support.
For individuals facing constraints due to a shortened upper arm bone (humerus), which hinders self-care tasks, surgical interventions aimed at lengthening the bone may be considered beneficial
Although there’s a slight increase in mortality rates among very young children with achondroplasia, once this initial period passes, their life expectancy matches that of any other child.
To ensure your child’s optimal well-being, it’s crucial to attend all well-baby checkups and annual appointments. These visits enable your child’s doctor to promptly address and manage any potential complications of achondroplasia, fostering your child’s thriving development. Additionally, these appointments provide you with the opportunity to discuss any questions or concerns you may have regarding your child’s growth and development.
Given the social and physical challenges that children with achondroplasia may encounter, facilitating connections with peers who share the condition can provide invaluable friendship, support, and guidance.
How is achondroplasia managed?
There is no cure for achondroplasia, but symptom management involves:
Regularly monitor infants’ height, weight, and head circumference for growth tracking.
Are there any treatments for achondroplasia?
While there is no cure, management focuses on:
Addressing potential complications, such as:
Weight management and promoting healthy eating habits to prevent obesity.
Surgical interventions like ventriculoperitoneal shunt for reducing brain fluid pressure or correcting craniocervical junction compression.
Adenoid and tonsil removal surgeries.
Administration of growth hormones.
Utilisation of continuous positive airway pressure (CPAP) nasal masks for apnea.
Ear tubes or antibiotics to prevent ear infections.
We are facilitating socialisation support.
Ongoing research explores medications that may enhance height by a few inches.
Prevention Measures
How can the risk of having a child with achondroplasia be minimised?
Preventing random cases is challenging because achondroplasia often stems from a rare genetic mutation. Preimplantation genetic testing can significantly reduce the likelihood of passing on the condition if a parent has achondroplasia. Consult your OB/GYN provider for further information.
Life Expectancy
What is the life expectancy of individuals with achondroplasia?
Most individuals with achondroplasia have a typical life span and average intelligence despite potential developmental delays in infancy. Although complications are possible, proactive symptom management can mitigate the risk of severe health issues later in life.