Rephrased Paragraph:
Wrist arthroplasty, or wrist joint replacement, is a less frequent procedure compared to knee or hip replacements but serves as a viable option for individuals suffering from severe arthritis that doesn’t improve with conventional treatments. During this surgery, the worn-out sections of the wrist bones are surgically removed and substituted with artificial implants designed to restore function and reduce pain.
Rephrased Content
Anatomy
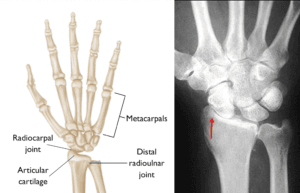
The wrist differs structurally from joints like the hip or knee. It connects the hand to the forearm through a complex arrangement of bones and joints. On the hand side, the wrist comprises two rows of carpal bones, with four bones in each row. These bones allow for motion within the wrist by shifting against one another. Beyond the carpal bones lie the metacarpals, which link the wrist to the fingers, providing a stable structure for hand movement.
The forearm consists of two bones: the radius and ulna, which form a joint with the first row of carpal bones. This joint is essential for flexing and extending the wrist. The radius, situated on the thumb side, is broader at the wrist compared to the ulna, which lies on the pinky side and is narrower. Additionally, the distal radioulnar joint, where the radius and ulna meet, plays a crucial role in forearm rotation.
At the ends of these bones, cartilage covers the joint surfaces, providing a smooth, elastic layer that facilitates seamless motion. Over time, however, this cartilage can deteriorate from regular use or suffer damage due to trauma or medical conditions like rheumatoid arthritis. When cartilage loss occurs, the result is arthritis, which can cause joint pain and impaired function.
Causes
Arthritis develops when cartilage in the joints wears away or becomes damaged, leading to direct contact and friction between the bones. This condition is often painful and can significantly impact joint function.
The most prevalent type, osteoarthritis, is characterized by the gradual erosion of cartilage over time, usually due to aging and extended use. In contrast, rheumatoid arthritis is an autoimmune disorder that triggers chronic inflammation, resulting in joint pain, stiffness, and swelling. It commonly affects multiple joints on both sides of the body.
Post-traumatic arthritis arises from injuries such as fractures or dislocations. Though similar to osteoarthritis in symptoms, it develops more rapidly following the traumatic event. All types of arthritis can weaken the wrist’s strength and mobility, limiting hand function.
Let me know if any specific SEO keywords need to be included or if further adjustments are needed!
Rephrased Content
Who Is a Suitable Candidate for Wrist Joint Replacement?
Individuals most likely to benefit from wrist joint replacement surgery typically experience severe arthritis but do not rely on their wrist for heavy physical demands in daily activities. The primary objectives of wrist replacement surgery include:
- Pain Relief: Alleviating chronic pain associated with arthritis.
- Function Maintenance: Preserving or enhancing wrist and hand function.
Currently available wrist joint replacement implants are less durable compared to those designed for hip, knee, or shoulder replacements. They are not suitable for patients with highly active lifestyles who frequently lift heavy weights. Instead, these implants are best suited for individuals whose daily activities place minimal stress on their wrists.
For those seeking to maintain an active lifestyle that includes heavy lifting, a wrist fusion may be a more appropriate option. This procedure eliminates motion at the wrist but typically results in a strong and pain-free joint capable of withstanding greater physical demands.
Your Surgery
Wrist replacement surgery aims to restore or enhance wrist mobility and improve the ability to perform daily activities, especially when arthritis affects the elbow and shoulder joints. In total joint replacement procedures, the damaged ends of the bones are excised and replaced with an artificial joint (prosthesis).
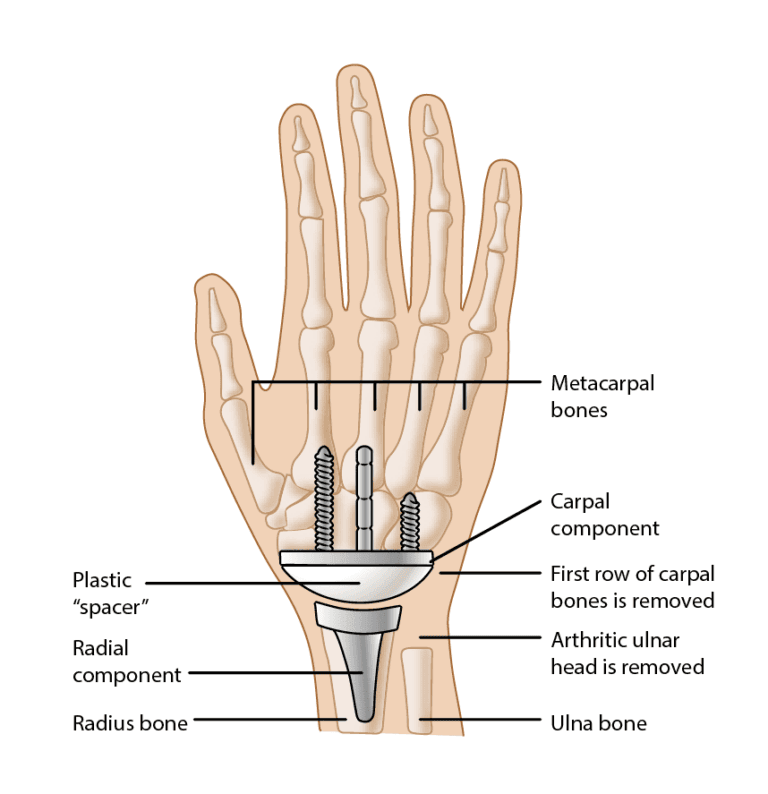
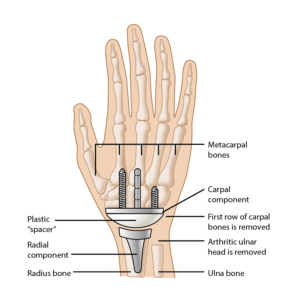
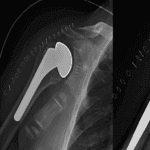
Implants
A variety of implant designs are available, most consisting of two components, each intended for one side of the joint. These components are primarily made of metal, with a high-quality plastic known as polyethylene serving as a spacer between them. Recent implant designs focus on closely replicating the wrist’s anatomical structure.
One component is inserted into the radius of the forearm, featuring a curved surface that aligns with a second component placed on the wrist side. The component that interfaces with the carpal bones has a flat surface directed toward the first component and is secured via a long stem and one or two shorter stems or screws.
The plastic spacer fits between the two components within the joint area and comes in various sizes to accommodate the patient’s wrist dimensions. Typically, one side of the spacer is flat while the other is rounded, allowing it to fit into the carpal component while enabling motion on the radial component.
Let me know if you need any additional changes or further assistance!
Rephrased Content
Procedure
Wrist joint replacement can typically be performed as an outpatient procedure, allowing patients to return home on the same day as the surgery. This surgery can also be combined with additional procedures aimed at correcting deformities or disorders affecting the tendons, nerves, and smaller joints in the fingers and thumb.
Here’s an overview of how the procedure is carried out:
- Incision: The surgeon begins by making an incision on the back of the wrist.
- Bone Removal: The arthritic ends of the lower arm bones are removed, and the surgeon may also excise the first row of carpal bones if necessary.
- Radial Component Insertion: The radial component of the prosthesis is inserted into the center of the radius bone, located on the thumb side of the forearm. This component is often secured in place with bone cement.
- Carpal Component Insertion: Depending on the design of the component, the surgeon then either inserts the carpal component into the center of the third metacarpal bone or screws it into the remaining row of carpal bones. Bone cement may also be used to secure this component, and the carpal bones may be linked or fused together for added stability.
- Spacer Placement: An appropriately sized polyethylene spacer is inserted between the metal components to allow for smooth motion.
- Closure: Once the components are in place, the surgeon closes the incision in the skin, and a splint is often applied to support the wrist during recovery.
If you have any additional requests or further sections to rephrase, feel free to share!
Rephrased Content
Recovery
After wrist joint replacement surgery, it is common to wear a splint or cast for several weeks to support the wrist during the initial healing phase. Although many patients experience quick pain relief, it’s essential to engage in gradual exercises through physical therapy over the following weeks. This rehabilitation process aims to restore movement and ultimately enhance strength and endurance.
The physical demands placed on the wrist prosthesis can influence the longevity of the implant, and certain limitations will need to be observed. For example:
- Tool Use: It is advisable to avoid using hammers or pneumatic tools.
- Weight Restrictions: Lifting heavy weights should be limited.
- Fall Prevention: Activities that could lead to falls should be avoided, as a fall on an outstretched hand can fracture the prosthesis, similar to a normal wrist injury.
Despite advancements in wrist prostheses, there is still a risk of loosening or failure due to wear or deformation. If these complications arise, additional surgical intervention may be necessary.
Outcomes
On average, wrist replacement surgery can restore approximately 50% of normal wrist motion and is expected to last between 10 to 15 years with proper care. Patients who do not adhere to post-surgical restrictions are at a higher risk of implant failure, underscoring the importance of careful patient selection to ensure optimal outcomes.
As with all implants, long-term follow-up appointments are recommended. Regular check-ups every one to two years allow your surgeon to monitor for any emerging conditions or complications.
If you need further revisions or additional sections to be rephrased, just let me know!