Transient osteoporosis of the hip is an uncommon condition characterized by temporary bone loss in the upper section of the thighbone (femur).
Individuals with this condition often experience a sudden onset of hip pain, which intensifies during walking or weight-bearing activities. Over time, this discomfort can escalate, potentially becoming severe enough to interfere with daily activities.
Fortunately, the painful symptoms usually subside gradually and disappear entirely within 6 to 12 months. In most cases, the affected hip regains its normal bone strength during the recovery process.
It’s important to note that transient osteoporosis of the hip is distinct from age-related osteoporosis. Unlike the progressive, painless bone weakening associated with age-related osteoporosis—which increases the risk of fractures throughout the body—transient osteoporosis is temporary and localized, with a defined recovery period.
Anatomy
The hip is one of the largest and most crucial joints in the human body, functioning as a ball-and-socket joint. The socket, known as the acetabulum, is part of the pelvic bone, while the ball is the femoral head, which forms the upper portion of the femur (thighbone). This structure allows for a wide range of motion and supports the body’s weight during activities such as walking and running.
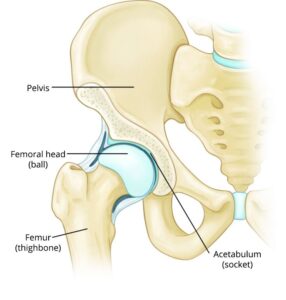 The hip is a ball-and-socket joint. In a healthy hip, the femoral head (ball) fits firmly into the acetabulum (socket).
The hip is a ball-and-socket joint. In a healthy hip, the femoral head (ball) fits firmly into the acetabulum (socket).