Rephrased Paragraph
Idiopathic scoliosis is a condition characterized by an abnormal sideways curvature of the spine, commonly seen in children and adolescents. While there are multiple forms of scoliosis, idiopathic scoliosis—where the cause remains unknown—is by far the most prevalent. The majority of idiopathic scoliosis cases emerge between the ages of 10 and skeletal maturity. Typically, scoliosis is painless, and mild curves often go unnoticed by both children and their parents until identified during routine screenings or pediatric check-ups.
In many instances, scoliosis requires no treatment as the spinal curvature is minor. However, for children with more pronounced curvatures, treatment may involve wearing a brace or undergoing surgery to help realign the spine and support proper posture.
Description
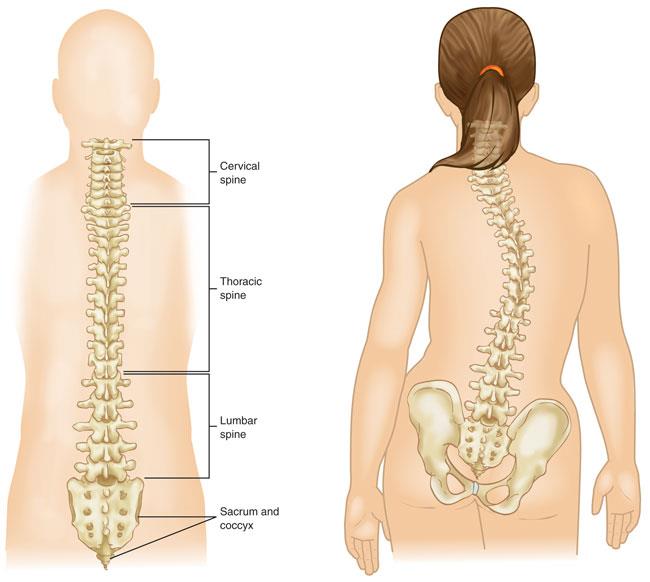
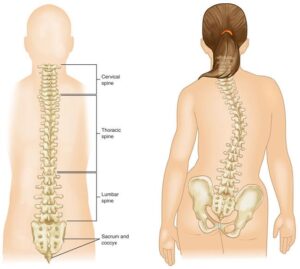
Scoliosis causes the spine’s vertebrae to twist or rotate, resulting in a curved alignment that resembles the shape of a “C” or “S” rather than following a straight line down the center of the back. These scoliosis curves frequently occur in the thoracic spine (upper and middle back), although they can also develop in the lumbar region (lower back) or even in both the upper and lower sections simultaneously.
Idiopathic scoliosis curves can vary in degree, with mild curves being more common than severe ones. Rapid curve progression may occur, particularly if the child experiences a growth spurt while still developing.
Although idiopathic scoliosis can develop in toddlers and young children, it most commonly appears during puberty. Both boys and girls are susceptible to scoliosis; however, girls are more prone to developing larger curves that may necessitate medical intervention.
Less common forms of scoliosis include:
- Congenital scoliosis: This form occurs when the spine’s vertebrae do not fully develop or fuse before birth, causing structural issues. Babies born with congenital scoliosis may have spinal abnormalities.
- Neuromuscular scoliosis: Scoliosis can result from neuromuscular conditions, such as muscular dystrophy or cerebral palsy, which impact the nerves and muscles. These conditions can weaken and unbalance the muscles that support the spine, contributing to the development of scoliosis.
Cause
The exact cause of idiopathic scoliosis remains unclear, but it is unrelated to specific habits or physical activities like carrying a heavy backpack or maintaining poor posture.
Research indicates a genetic component, as approximately 30% of adolescents with idiopathic scoliosis have a family history of the condition.
Symptoms
Mild scoliosis curves may remain undetected until a child undergoes a growth spurt during puberty, at which point more visible signs may appear, such as:
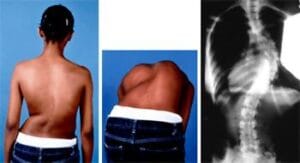
- Uneven shoulders, with one shoulder blade more prominent than the other
- Rib prominence on one side of the body
- Asymmetrical waistline
- One hip positioned higher than the other
As many adolescents may feel self-conscious and prefer loose clothing, scoliosis is often first identified during school screenings or routine pediatric exams.
If a pediatrician suspects scoliosis, they may refer the child to a pediatric orthopedic surgeon or a spinal deformity specialist for comprehensive evaluation and a personalized treatment plan.
Doctor Examination
Physical Examination
A common screening test for scoliosis is the “Adam’s forward bend test.” In this test, the child bends forward with feet together, knees straight, and arms relaxed. The doctor observes from behind, examining the symmetry of the rib shape on each side, as any spinal curvature becomes most visible in this position.
While the child stands upright, the doctor will also assess the alignment of the hips and shoulders and ensure the head is centered over the hips. Additionally, the doctor will evaluate the range of spinal movement in all directions.
To exclude other potential causes of spinal curvature, the doctor will check for differences in limb length, abnormal neurological signs, and other physical factors.
X-rays
X-rays provide detailed images of the spinal bones, helping the doctor identify the precise location and severity of the curve. This imaging allows for accurate measurement, as curves exceeding 25 degrees typically warrant treatment, depending on the child’s age and growth potential.
Treatment Options
When developing a treatment plan for your child’s scoliosis, the doctor will take into account several factors, including:
- The curve’s location
- The curve’s severity
- The child’s age
- Remaining growth potential—since scoliosis curves are less likely to progress rapidly after full skeletal maturity.
By assessing these elements, the doctor can estimate the likelihood of curve progression and recommend the most effective treatment approach.
Nonsurgical Treatment
- Observation: For spinal curves under 25 degrees or when a child is nearing full growth, the doctor may suggest periodic monitoring to ensure the curve does not worsen. Follow-up appointments, typically every 6 to 12 months, will include X-rays to track the spine’s development until growth is complete.
- Bracing: If the spinal curve ranges from 25 to 45 degrees and the child is still growing, bracing may be advised. Although a brace will not correct an existing curve, it can often prevent further progression, potentially avoiding the need for surgery.
Research has shown that bracing can significantly reduce the likelihood of curve progression to a surgical level, especially in patients with curves at high risk of worsening.
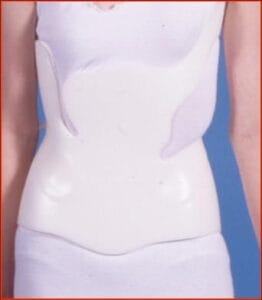
There are various brace designs for scoliosis, most of which are custom-fitted underarm braces tailored to the child’s body for comfort. The doctor will recommend the most suitable brace type and specify the daily wear time. Loose-fitting clothing can easily conceal the brace, and children may remove it for sports or other physical activities.
Surgical Treatment
Spinal Fusion
If your child’s spinal curve exceeds 45 to 50 degrees or if bracing has not prevented the curve from progressing to this degree, surgery may be recommended. Untreated severe curves can continue to worsen and may eventually compromise lung function.
The surgical procedure known as spinal fusion can significantly straighten the spinal curve and then fuse the affected vertebrae, allowing them to heal into a single, solid bone. This fusion halts further growth in the section of the spine impacted by scoliosis.
During the procedure, the misaligned vertebrae are carefully repositioned. Bone grafts, consisting of small bone pieces, are placed between the vertebrae intended for fusion. Over time, these bones grow together, similar to the healing process of a fractured bone.
To maintain alignment during healing, metal rods are typically used to stabilize the spine. These rods are secured to the spine with hooks, screws, or wires.
The extent of spinal fusion depends on the specific curve(s) present in the child’s spine. Only the affected vertebrae are fused, preserving mobility in the unaffected parts of the spine to support natural movement.
Alternative Procedures
Some medical institutions are exploring fusion-less spine surgery for younger patients with moderate scoliosis curves (45 to 50 degrees) who are still growing. This technique, known as tethering growth modulation surgery, aims to guide spine growth without fusion. However, further patient follow-up is needed to assess its long-term effectiveness and durability. Due to this need for more data, spinal fusion remains the gold standard in surgical treatment for scoliosis.
Recovery
Most patients are able to walk without a brace by the first day after spinal fusion surgery. Hospital discharge generally occurs 3 to 4 days post-surgery. Children can typically return to school and resume daily activities within four weeks.
Long-Term Outcomes
Spinal fusion surgery is highly effective in preventing further curvature progression and significantly straightening the spine, enhancing physical appearance.
Within 6 to 9 months post-surgery, most children can return to sports activities, although permanent limitations on certain spine movements may restrict participation in high-impact contact sports like football.
Importantly, spinal fusion surgery does not increase the risk of complications during future pregnancies or deliveries for girls.