Patellofemoral arthritis occurs when the cartilage beneath the kneecap (patella) and the groove in the thighbone (femur) where it glides become damaged or worn. This condition often leads to discomfort at the front of the knee and can significantly hinder daily movements such as kneeling, squatting, and navigating stairs, particularly descending.
Anatomy
The patella, commonly known as the kneecap, is a small bone positioned at the front of the knee joint where the thighbone (femur) and shinbone (tibia) meet. Its primary role is to shield the knee and serve as a crucial connection between the thigh muscles and the tibia.
This bone rests within a specialized groove on the femur, known as the trochlear groove. As the knee bends and straightens, the patella glides smoothly within this groove.
The ends of the femur, the trochlear groove, and the underside of the patella are all covered by a smooth, lubricating layer called articular cartilage. This cartilage ensures that the bones move effortlessly against one another during leg movements, minimizing friction and preventing damage.
 (Left) The patella rests in a small groove at the end of the femur called the trochlear groove. (Right) As you bend and straighten your knee, the patella slides up and down within the groove.
(Left) The patella rests in a small groove at the end of the femur called the trochlear groove. (Right) As you bend and straighten your knee, the patella slides up and down within the groove.
Description
Patellofemoral arthritis arises when the articular cartilage beneath the patella and along the trochlear groove deteriorates and becomes inflamed.
As the cartilage wears down, it can develop a rough, frayed texture. In severe cases, the underlying bone becomes exposed. Movement along these uneven surfaces can result in significant pain, especially as the bones rub against each other.
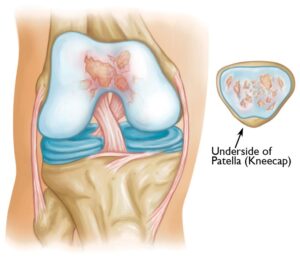 Illustration shows patellofemoral arthritis. The patella (kneecap) has been removed to show damage to the cartilage on the underside.
Illustration shows patellofemoral arthritis. The patella (kneecap) has been removed to show damage to the cartilage on the underside.
 (Left) This X-ray shows a normal knee from the side. The arrows point to the normal amount of space between the bones. (Middle) In this X-ray, the arrows point to narrowed joint space due to patellofemoral arthritis. (Right) Here, the arrows point to bone spurs that have developed due to the arthritis.
(Left) This X-ray shows a normal knee from the side. The arrows point to the normal amount of space between the bones. (Middle) In this X-ray, the arrows point to narrowed joint space due to patellofemoral arthritis. (Right) Here, the arrows point to bone spurs that have developed due to the arthritis.Cause: Dysplasia
Dysplasia refers to a condition where the patella (kneecap) is not properly aligned within the trochlear groove of the femur. This misalignment increases stress on the cartilage during knee movement, leading to accelerated wear and tear. Over time, this added strain can cause the cartilage to deteriorate, potentially contributing to the development of patellofemoral arthritis.
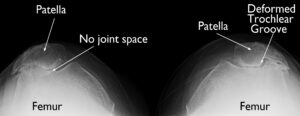 X-ray taken from above the knee shows dysplasia that has developed into severe arthritis. There is no joint space remaining in the knee on the left. On the right, the trochlear groove has become deformed.
X-ray taken from above the knee shows dysplasia that has developed into severe arthritis. There is no joint space remaining in the knee on the left. On the right, the trochlear groove has become deformed.
Kneecap Fracture
A fracture of the patella (kneecap) often results in damage to the articular cartilage that lines the underside of the bone. Even after the fracture heals, the joint surface may remain uneven. This irregularity creates friction as the patella moves along the femur, which can progressively lead to arthritis over time.
Symptoms
The most prominent symptom of patellofemoral arthritis is knee pain, specifically at the front of the knee where the patellofemoral joint is located. While the pain can sometimes occur at rest or without any activity, it is more commonly triggered by activities that put pressure on the kneecap, such as kneeling, squatting, climbing or descending stairs, and standing up from a low chair.
Another symptom is a crackling or grinding sensation, known as crepitus, which can occur when moving the knee. This sensation may sometimes be painful and loud enough to be audible to others. In advanced cases, the kneecap may catch or lock when the knee is straightened, making movement difficult.
Doctor Examination
Medical History
During a medical consultation, your doctor will gather detailed information about your general health, knee pain, and daily functional abilities.
They will focus on pinpointing the location of the pain, which is often behind the kneecap or at the front of the knee (anterior knee pain). Patients typically report discomfort during activities that put stress on the kneecap, such as:
- Climbing or descending stairs
- Sitting with the knee bent for long periods
- Rising from a seated position
Physical Exam
The physical examination involves assessing the knee in various positions to identify pain, stiffness, or restricted movement. Your doctor will also check for signs such as crepitus (a grinding noise indicating bone-on-bone contact), muscle weakness (atrophy), and damage to surrounding tissues, including muscles, tendons, and ligaments.
Key steps in the exam include:
- Inspecting the knee’s alignment to assess joint stability
- Palpating (feeling) the knee to reproduce pain and identify tender areas
- Testing the knee’s range of motion to detect stiffness or abnormal patellar tracking (displacement of the kneecap during movement)
- Evaluating ligament strength and overall knee stability
Imaging Tests
- X-rays: X-rays are used to visualize the bones and determine whether arthritis is localized to the patellofemoral joint. Multiple angles are captured to evaluate joint alignment.
- MRI Scans: An MRI provides detailed images of soft tissues, allowing the doctor to assess the condition of the cartilage more precisely.
Treatment
Nonsurgical Options
Most cases of patellofemoral arthritis can be managed without surgery. Common nonsurgical treatments include:
- Nonsteroidal Anti-Inflammatory Drugs (NSAIDs): Medications like aspirin, ibuprofen, or naproxen reduce pain and inflammation.
- Exercise: Low-impact activities, such as walking and swimming, help reduce stiffness and strengthen supporting muscles. Avoid high-impact exercises or activities that stress the kneecap, such as squatting.
- Activity Modification: Reducing or avoiding activities that exacerbate symptoms, like climbing stairs, can help manage pain.
- Weight Loss: Losing excess weight reduces stress on the knee, easing symptoms and improving mobility.
- Physical Therapy: Specific exercises, such as those that strengthen the quadriceps, can relieve pressure on the kneecap. A physical therapist can guide a tailored exercise plan.
- Cortisone Injections: Steroid injections deliver powerful anti-inflammatory effects directly to the knee joint.
- Viscosupplementation: This procedure involves injecting a gel-like substance into the joint to improve lubrication. Its effectiveness is still being studied.
Surgical Treatment
When nonsurgical methods are ineffective, surgical intervention may be recommended. Surgical options include:
- Chondroplasty: Using arthroscopy, a surgeon trims and smooths rough cartilage surfaces to reduce friction.
- Realignment: Soft tissues surrounding the kneecap are adjusted to improve its position within the trochlear groove.
- Cartilage Grafting: Healthy cartilage is transplanted to damaged areas, often suitable for younger patients with localized cartilage loss.
- Tibial Tuberosity Transfer: This procedure shifts the attachment point of the patellar tendon to alter kneecap positioning, reducing joint stress.
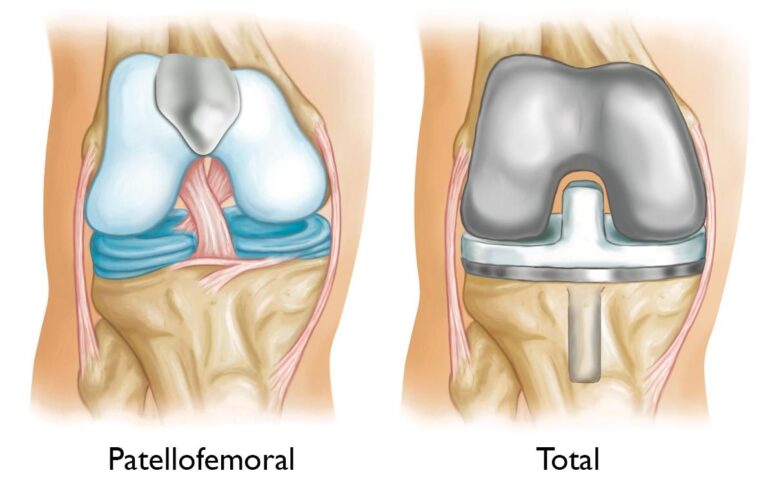
- Patellofemoral Replacement: In partial knee replacement, the damaged cartilage and a small portion of bone are removed and replaced with prosthetic components. These components are secured with cement and restore smoother movement in the joint.
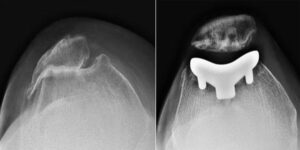 (Left) X-ray taken from above the knee. The patella and the trochlear groove of the femur have become deformed due to arthritis. There is bone rubbing on bone. (Right) The same knee after patellofemoral replacement. The patellar implant on the underside of the kneecap does not show in an X-ray.
(Left) X-ray taken from above the knee. The patella and the trochlear groove of the femur have become deformed due to arthritis. There is bone rubbing on bone. (Right) The same knee after patellofemoral replacement. The patellar implant on the underside of the kneecap does not show in an X-ray.
Patellofemoral replacement surgery is not suitable if arthritis affects other parts of the knee. In such cases, your doctor may recommend a total knee replacement to address the issue comprehensively.
Total Knee Replacement
A total knee replacement involves resurfacing all the cartilage-covered areas within the knee joint. During the procedure:
- The end of the femur and the top of the tibia are fitted with metal prosthetic components.
- A plastic spacer is inserted between these components to provide a smooth surface for joint movement.
- The patella is typically resurfaced with a plastic button to ensure seamless motion and minimize friction.
This approach is designed to relieve pain, restore joint functionality, and improve mobility for patients with widespread arthritis in the knee.
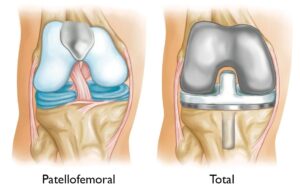 (Left) Patellofemoral replacement. This partial knee replacement can be used to treat arthritis that is limited to the underside of the patella and the trochlear groove. If other parts of the knee are involved, a total knee replacement (Right) may be recommended.
(Left) Patellofemoral replacement. This partial knee replacement can be used to treat arthritis that is limited to the underside of the patella and the trochlear groove. If other parts of the knee are involved, a total knee replacement (Right) may be recommended.
Outcomes
Treatment for patellofemoral arthritis is generally effective in alleviating pain and enhancing knee function for most patients. However, the success of treatment can vary based on individual factors such as the severity of the condition, overall health, and the specific type of treatment pursued. Your doctor will discuss the likely outcomes and set realistic expectations tailored to your unique situation.
To support healthcare providers in managing osteoarthritis of the knee without surgery, the American Academy of Orthopaedic Surgeons (AAOS) has conducted extensive research and developed evidence-based guidelines to optimize patient care.