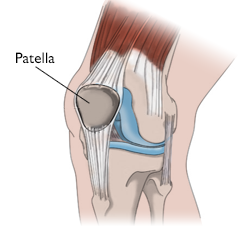
When your patella, or kneecap, stays properly aligned within the trochlear groove of your knee joint, movement feels seamless—allowing you to walk, run, sit, and stand with ease. However, when the kneecap shifts out of this groove, it can lead to recurrent instability, where frequent dislocations occur, accompanied by pain and discomfort.
Anatomy of Kneecap Instability: Key Structures and Risk Factors
The patella, or kneecap, connects the thigh muscles to the shinbone (tibia), playing a vital role in knee movement. During leg bending or straightening, the kneecap moves up and down, guided by the V-shaped femoral groove at the end of the thighbone (femur). This alignment is stabilized by multiple restraints, including ligaments, muscles, and bone structures, ensuring the patella stays in the trochlear groove.
However, several factors can increase the likelihood of the kneecap shifting out of its proper position:
- Medial Patellofemoral Ligament (MPFL) Damage: This ligament prevents the patella from moving excessively sideways. Its damage can lead to instability.
- Flattened Trochlear Groove: A groove that is too shallow may fail to securely hold the patella in place.
- Abnormal Limb Alignment: Conditions like being “knock-kneed” or having atypical bone alignment can shift the patella out of position.
- Rotational Abnormalities: Irregular rotation of the femur or tibia can displace the kneecap.
- Misaligned Patellar Tendon Attachment: If the tendon connecting the patella to the shinbone is attached too far to the outer side of the knee, it can pull the kneecap out of the groove.
Causes of Patellar Dislocation
Patellar dislocation often occurs due to non-contact injuries, such as sudden pivots, twists, or awkward falls. Additionally, a direct blow to the kneecap can dislodge it from its position.
Symptoms of Kneecap Instability
Individuals with patellar instability may experience the following symptoms:
- Apprehension: A sensation that the kneecap is about to dislocate or move out of position.
- Kneecap Dislocations: Episodes where the kneecap actually shifts out of place.
- Pain and Swelling: Discomfort caused by damage to cartilage behind the kneecap.
By understanding the anatomy and factors contributing to patellar instability, individuals can better recognize and address this condition.
Medical Evaluation and Treatment Options for Kneecap Instability
Doctor’s Examination
Physical Examination
During your consultation, the doctor will conduct a thorough physical examination, which may include:
- Observing how you walk to assess gait abnormalities.
- Evaluating your knee’s range of motion by asking you to straighten and bend it.
- Examining the area around your kneecap to check for bone misalignment or muscle weakness in the thigh.
Imaging Tests
To confirm a diagnosis and assess the extent of the condition, the doctor may order imaging tests such as:
- X-rays: To identify alignment issues or structural abnormalities.
- MRI scans: To detect loose bone or cartilage fragments and evaluate ligament and knee anatomy.
- CT scans: Occasionally used when precise measurements of bone alignment are necessary.
Treatment Options for Kneecap Instability
Reduction for Dislocations
If the kneecap has been completely dislocated from the groove, the first priority is repositioning it, a process known as reduction. In some cases, reduction happens spontaneously without intervention. Otherwise, the doctor may gently guide the kneecap back into place.
Dislocations can damage the underside of the kneecap and the end of the thighbone, potentially leading to pain and arthritis over time.
Nonsurgical Treatments
For first-time dislocations, nonsurgical methods are often effective. These may include:
- Exercise Programs: Targeted exercises to strengthen thigh muscles and promote proper kneecap alignment.
- Bracing: Using a stabilizing brace to support the knee during recovery.
- Cycling: Low-impact cycling is frequently recommended as part of physical therapy to rebuild strength.
Patients can typically resume normal activities within 1 to 3 months with these treatments.
Surgical Treatments
For cases of recurrent instability or severe misalignment, surgery may be necessary. Surgical interventions might include:
- Reinforcing or balancing the soft tissue restraints, such as the ligaments keeping the kneecap in place.
- Correcting bone misalignments that contribute to instability.
- Reshaping the trochlear groove to better accommodate the kneecap.
Surgical treatment also reduces the risk of cartilage damage, which is a common concern with recurring instability.
Expected Outcomes
Nonsurgical Management
For first-time dislocations, nonsurgical approaches often yield excellent results, with a relatively low recurrence rate. However, patients with certain risk factors may face a higher chance of recurring dislocations.
Surgical Management
Surgical procedures generally have very positive outcomes, with re-dislocation rates of less than 10%. Surgery is typically reserved for:
- Patients with a high risk of re-dislocation after a first-time injury.
- Individuals with ongoing instability or recurrent dislocations.
- Cases involving severe patellar misalignment (maltracking) during movement.
Effective treatment, whether nonsurgical or surgical, can significantly improve knee function and quality of life for patients dealing with kneecap instability.